Systemic Sclerosis Associated with Alterations in Sub-Populations of B Cells
In a new study entitled “Systemic Sclerosis Patients Present Alterations in the Expression of Molecules Involved in B-Cell Regulation,” a team of researchers investigated whether patients with systemic sclerosis present changes in their immune B cells profile (including frequency and activation phenotypes), focusing particularly on the B cell subpopulation of transitional, naïve and memory B cells. They identified key abnormalities that may impact B cells hyperactivation in systemic sclerosis. The study was published in the journal Frontiers in Immunology.
Systemic sclerosis (SSc) is a systemic autoimmune disease characterized by excessive deposition of collagen, leading to skin thickening and affecting key organs, including the kidneys, heart, lungs and gastrointestinal tract. The fibrosis process in SSc patients is characterized by differentiation of tissue fibroblasts to myofibroblasts – in response to injury fibroblasts differentiate into contractile and secretory myofibroblasts to repair the tissue. However, this process can severely impair organ function when the production of extracellular matrix components (such as collagen) is excessive.
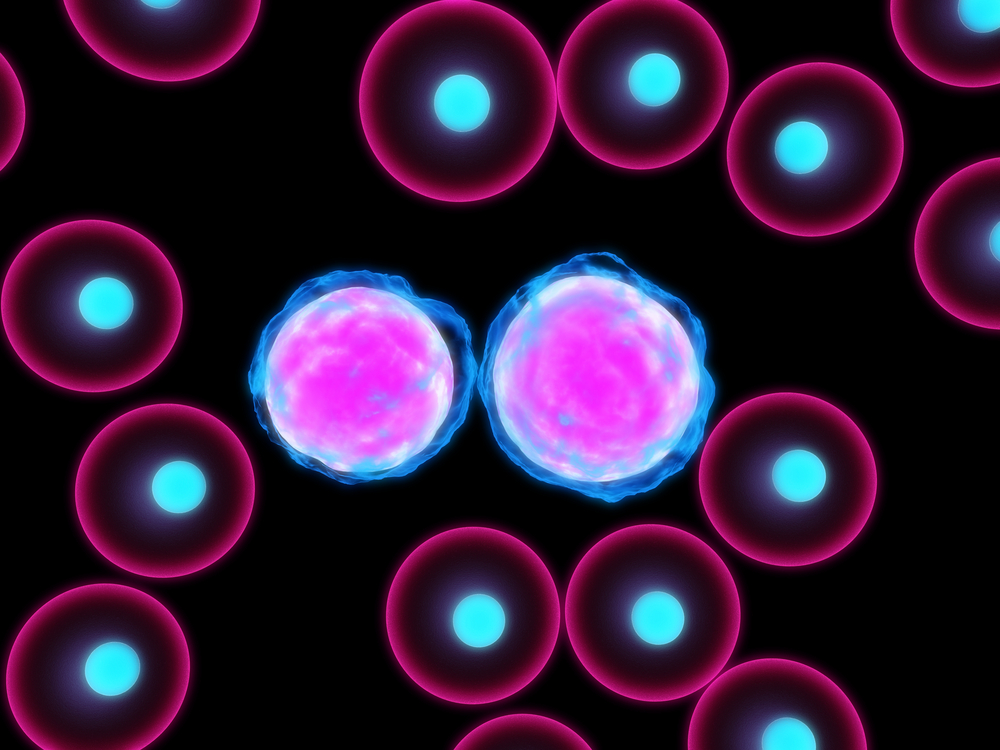
A recent report suggested that SSc patients exhibit a higher infiltration of a group of immune cells – called B cells – indicating a potential role for these cells in the pathogenesis of SSc. Increasing evidence supports a role of B cells in systemic autoimmune diseases – via antigen presentation to T cells and secretion of proinflammatory cytokines. More recently, however, some studies identified sub-populations of B cells, such as IL-10-producing B cells, carrying the ability to suppress autoimmune responses in humans. This group is part of the so-called transitional B cells, a group of immature B cells whose numbers and functions were found perturbed in systemic autoimmune diseases.
In this new study, authors investigated several parameters and the functional role of B cell subpopulations (including transitional, naive, and memory B cells) from SSc patients when compared to those from healthy individuals. Specifically, the team analyzed cells’ frequency, phenotype and expression of activating and inhibitory receptors between both conditions. To this end, the team retrieved blood samples from 31 patients with SSc (meeting the American College of Rheumatology criteria for SSc) and 53 healthy individuals.
Authors found significant alterations in the frequency of several B cell subpopulations in SSc patients. These changes were accompanied by disturbances in the ratio between activating and inhibitory factors. Specifically, the team discovered SSc patients’ exhibited a higher number of transitional and naive B cells, in relation to memory B cells. Additionally, naive and transitional B cells from SSc patients’ exhibited an activated phenotype, when compared to healthy controls.
This B cell activation may contribute to SSc pathogenesis, potentially by activating other cells of the immune system that lead to the production of profibrotic cytokines by fibroblasts. The research team is continuing this study to try to understand how the identified abnormalities in B cells affect their function and impact SSc pathology.