Innate Immunity Protein a Potential Therapeutic Target in Scleroderma, Study Suggests
Written by |
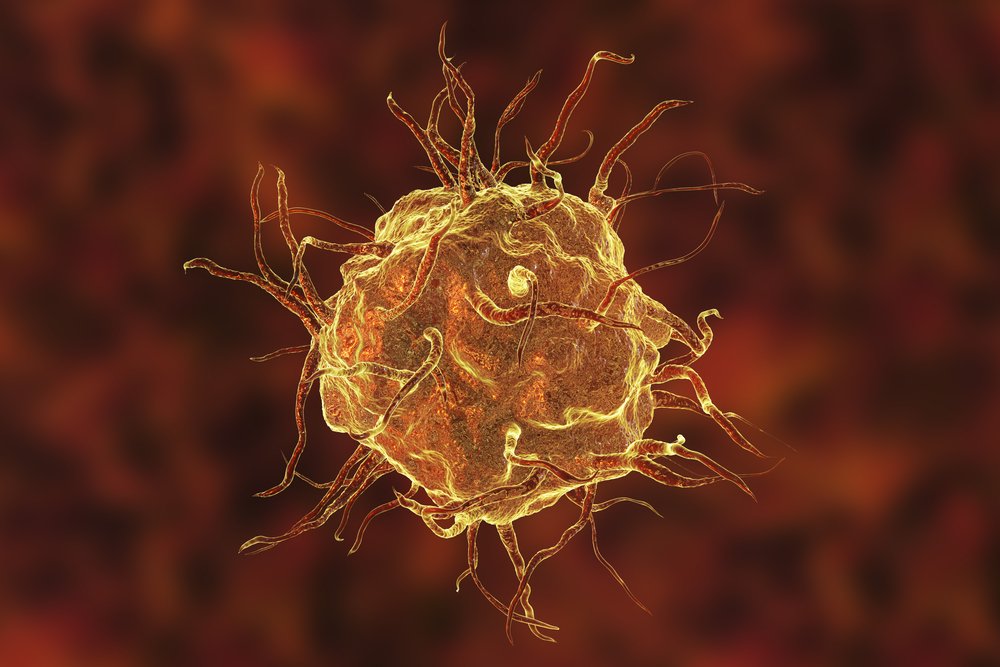
A key innate immunity protein called TLR4 is a key driver of organ fibrosis, according to a new study conducted in mice and scleroderma patients. The finding suggests that targeting TLR4 may be an effective therapeutic strategy in certain patients.
The study, “TLR4-dependent fibroblast activation drives persistent organ fibrosis in skin and lung,” was published in the journal JCI Insight.
Fibrosis (scarring) is a hallmark of scleroderma. Although what drives the variable extent and activity of fibrosis in this disease remains largely unknown, dysregulation of the innate immune system has been proposed as a key contributor.
TLR4 is a member of the TLR protein family that plays a crucial role in the activation of innate immunity (the first line of defense) against microbial pathogens. TLRs also recognize damage-associated molecule patterns (DAMPs), which act as signals to promote and exacerbate inflammatory response in noninfectious injuries.
Among the DAMP proteins that bind to TLR4 are components of the extracellular matrix, which provides structural and biochemical support to cells and is an essential driver of fibrosis.
As dysregulated cellular signaling mediated by TLR4 has been implicated in chronic inflammatory diseases, scientists have been studying ways to selectively inhibit this protein.
But attempts with a TLR4 inhibitor in clinical trials of sepsis (a potentially life-threatening complication from an infection) failed to show clinical effectiveness. And even less is known about the therapeutic potential of blocking TLR4 in scleroderma and other chronic fibrotic conditions.
The research team previously showed that fibrotic skin and lungs of scleroderma patients had higher levels of specific DAMPs, and that they were present in TLR4-containing myofibroblasts — a cell type that releases collagen during the development of fibrosis.
In mice, the genetic removal of two DAMPs eased skin and lung fibrosis. Also in studies with mice, the absence of functional TLR4 protected the animals from experimentally induced fibrosis.
The scientists studied whether cellular signaling through TLR4 is altered in scleroderma, and assessed the therapeutic potential of selective TLR4 targeting in fibrosis. They also evaluated if — like infectious pathogens — DAMPs require the formation of a complex between TLR4 and the receptor MD2 for their function.
Results showed that the levels of MD2 and TLR4 messenger RNA — which contains the information to make proteins — were increased in skin biopsies from scleroderma patients. In a subset of patients, the scientists also found higher levels of TLR4-responsive genes, or gene signatures, related to inflammation and wound healing.
Then they developed a small molecule that selectively blocks MD2. This approach eliminated pro-fibrotic responses in petri dishes and in patient-derived skin cells.
Importantly, the TLR4 inhibitor prevented and reversed organ fibrosis in several mouse models. The data also revealed that the genetic deletion of TLR4 in fibroblasts — cells with functional similarities to myofibroblasts and whose activation underlies severe skin and lung fibrosis in scleroderma — led to marked protection from skin and lung fibrosis.
“Together, results from these human and mouse studies implicate MD2/TLR4-dependent fibroblast activation as a key driver of persistent organ fibrosis,” the investigators wrote.
“The results suggest that [scleroderma] patients with high TLR4 activity might show optimal therapeutic response to selective inhibitors of MD2/TLR4 complex formation,” they added.





