DAY 19 Scleroderma Awareness Month: CALCINOSIS

DAY 19 Scleroderma Awareness Month: CALCINOSIS
Today’s topic is the debilitating, painful symptom of calcinosis.
It is important to note that not every scleroderma patient will experience calcinosis, since no two scleroderma patients present with the exact same set of symptoms. Calcinosis is more prevalent in the diffuse subset of scleroderma. The intake of calcium in the diet does not have a direct correlation with calcinosis.
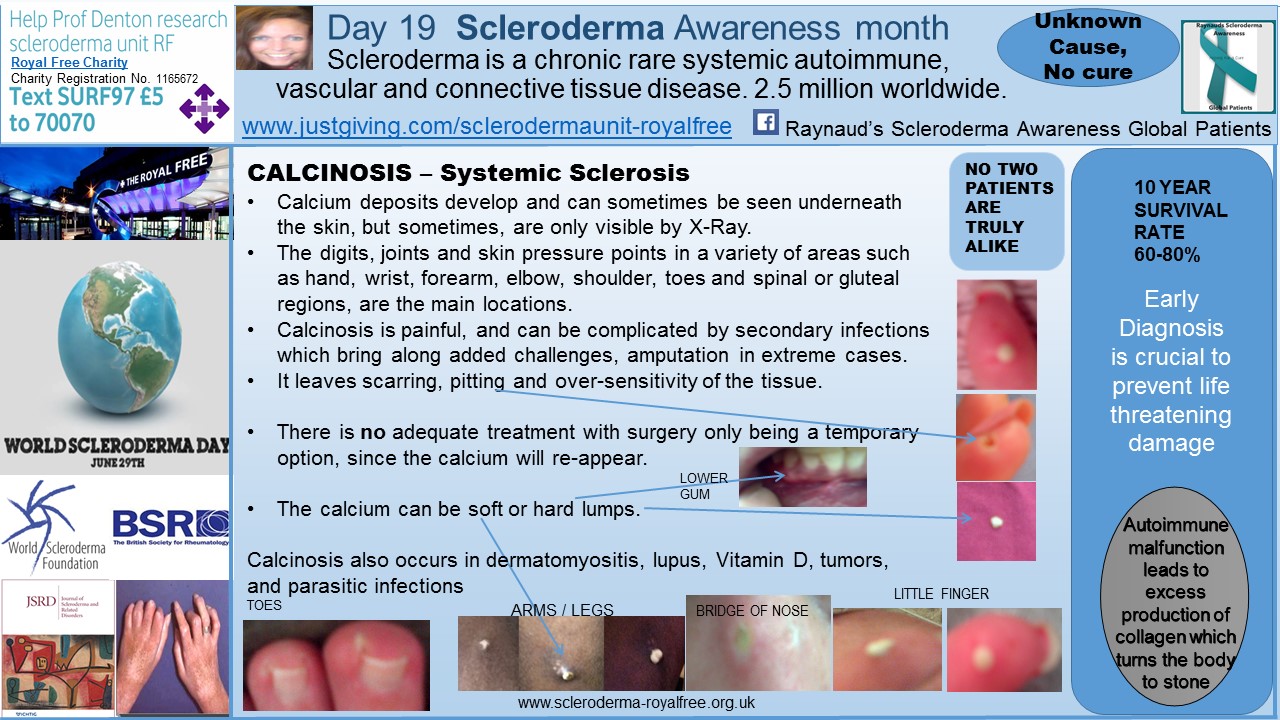
As can be seen in the diagram, calcinosis is not specific to certain areas of the body, it can appear anywhere, but usually, at sites of soft tissue injury or pressure points, which includes the gums.
The lumps of solid calcium can lie underneath the skin, being visible only by X-Ray, and are hard to touch, if near the outer surface.
Calcinosis is extremely painful, especially with tight, scleroderma-like skin. The lumps will eventually work themselves to the surface of the skin, where they can be pushed out. This process can take years. Added complications can occur if the area becomes infected, requiring antibiotic intervention. Which of course, brings along added gastro-intestinal challenges.
In my experience, the excision of a calcium lump is extremely painful, leaving a hole in the flesh from where the lump has been. On a few occasions I have almost passed out with the pain when a lump finally becomes loose and can be removed, leaving a huge hole which eventually fills with blood. Deep breaths, help at this point!
Removal is no guarantee that the calcium will be gone forever from that site, as the removal site can form more calcium. I have pitting and scars around my knees, nose, elbows, toes and fingers from where calcium lumps have been.
The calcium can also be a soft, chalky-like liquid underneath the skin, which can be excruciatingly painful, if touched. Similar, to the lumps of calcium, the softer lumps can take years to work themselves to the surface of the skin for removal. This process being hindered by tight skin and a compromised immune and circulatory system, due to the nature of the scleroderma disease process.
Although calcinosis is not a direct life threatening symptom when comparing to severe internal organ involvement such as heart failure or renal crisis, it is a huge unmet need of the scleroderma patient.
Currently, there are no adequate treatments or medications for calcinosis. Some patients report a marginal improvement when taking the antibiotic Minocycline, but personally, I saw no improvement. I have also spoken with patients who had undergone surgery for calcium removal, with the calcium only returning in time. I am not brave enough for this option being a reality for me!
On a personal observational level, the calcium lump or liquid appears as sites of injury and pressure points, with tight skin, adding to the make-up ingredients. I have also noticed that Raynaud’s episodes / blue fingers and toes can help the calcium forming.
Prof. Herrick and her team at Salford Royal Hospital in Manchester, here in the UK, have a special interest in calcinosis research. With their most recent publication being published in the Scandinavian Journal of Rheumatology at the start of the year, concluding that
‘The thumb is affected by calcinosis more than other digits, followed by the index finger. This observation provides insight into the pathogenesis of SSc-related calcinosis, which may relate more to repetitive trauma than to ischaemia.’
To learn more about Prof Herrick and her team, click here.
In my view, investment in research is needed as a matter of emergency to investigate the formation of solid calcium / bone-like lumps taking over scleroderma patient body.
I am very much hoping that the Factor XIII trial being carried out by the clinical trials team at the Royal Free Hospital will reveal the calcinosis antidote.
To read my blog post about this, see: Day 13 SclerodermaAwareness Month, click here.
Note: Scleroderma is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this blog article are not those of Scleroderma News and are only intended to spark discussion about issues pertaining to the disease.