Woman, 79, found to have rare case of localized scleroderma
Clinicians highlight importance of full patient screening in study
Written by |

Clinicians in Tunisia highlighted the importance of screening for self-reactive antibodies, or autoantibodies, in localized scleroderma cases after a 79-year-old woman treated a hospital in the capital city of Tunis was also diagnosed with pulmonary interstitial fibrosis and pulmonary arterial hypertension.
In addition, the patient had self-reactive anti-Th/To antibodies, according to the case report.
In their report, the researchers stressed the importance of screening for autoantibodies, such anti-Th/To, in patients with severe localized scleroderma and when other autoimmune diseases are suspected.
Also, “extracutaneous involvement may be predicted based on clinical findings and autoantibody profiles,” they wrote.
The case study, “Localized scleroderma with pulmonary arterial hypertension and pulmonary interstitial fibrosis in a patient with positive Th/to antibodies: Case report and review of literature,” was published in the journal Clinical Case Reports.
5th reported case of morphea patient with respiratory issues
Localized scleroderma, also known as morphea, is characterized by thick and hard patches of skin due to the accumulation of collagen, a protein the body normally uses to repair wounds.
This form of scleroderma rarely affects internal organs. As such, it is distinct from the systemic form of the disease, which presents specific autoantibodies, multiple organ dysfunction, and Raynaud’s phenomenon — when fingers and toes feel numb and prickly under cold or stress.
In this case report, researchers in the North African country described a rare case of generalized localized scleroderma. The case was defined by the presence of widespread patches of thickened skin, associated with pulmonary interstitial fibrosis, pulmonary arterial hypertension, and Th/To autoantibodies — antibodies that mistakenly attack the body’s own tissues.
The patient sought treatment after experiencing itchy and diffuse hard skin for three months. On physical examination, she was found to have areas of darkened skin and wasting of the trunk. The hardened patches of skin were located on the chest, abdomen, and back, but not the extremities.
The woman had no digital ulcerations, no discoloration of her fingers and toes when exposed to cold, and no shortness of breath, difficulty swallowing, joint pain, or other systemic symptoms.
A skin biopsy revealed the presence of thick collagen bundles, and a reduction in adnexal structures — those involved in protecting and/or supporting the function of an organ. One type of sweat glands were smaller than normal and closed off by newly formed collagen.
Overall, the clinical findings and skin biopsy led to a diagnosis of generalized localized scleroderma. Blood testing was positive for anti-Th/To antibodies. However, antibodies specific to systemic scleroderma were not present.
The woman was treated with systemic prednisone and topical steroids for two months, which led to a very slight improvement.
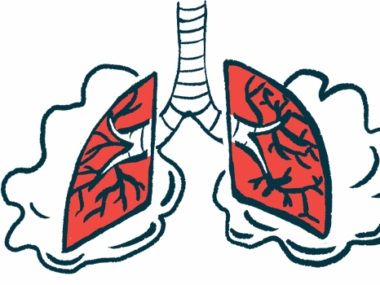
Further X-ray and CT scan examinations revealed the presence of pulmonary interstitial fibrosis, also known as interstitial lung disease (ILD), a group of disorders characterized by lung inflammation and scarring, called fibrosis. ILD is a leading cause of death among people with scleroderma.
To the best of our knowledge, our patient represents the fifth reported case of [generalized localized scledoderma] with a respiratory involvement consisting of lung fibrosis.
Echocardiography — a way of imaging the heart — helped detect pulmonary arterial hypertension, or PAH, which is high blood pressure in the arteries of the lungs. PAH is a condition frequently associated with scleroderma.
These findings led to a final diagnosis of localized scleroderma with pulmonary interstitial fibrosis and PAH. Treatment with a monthly intravenous (into-the-vein) dose of cyclophosphamide, an immune system suppressant, was started.
“To the best of our knowledge, our patient represents the fifth reported case of [generalized localized scledoderma] with a respiratory involvement consisting of lung fibrosis,” the researchers wrote.
“The presence of anti-Th/To antibodies may constitute the pathophysiological [disease mechanisms] substratum of the fibrosing lung disease and the association of morphea and [pulmonary interstitial fibrosis] may be so attributed to concurrent autoimmune diseases,” they added.