Study Suggests High-Resolution Computed Tomography as a Predictor of Lung Function in Systemic Sclerosis Patients
Written by |
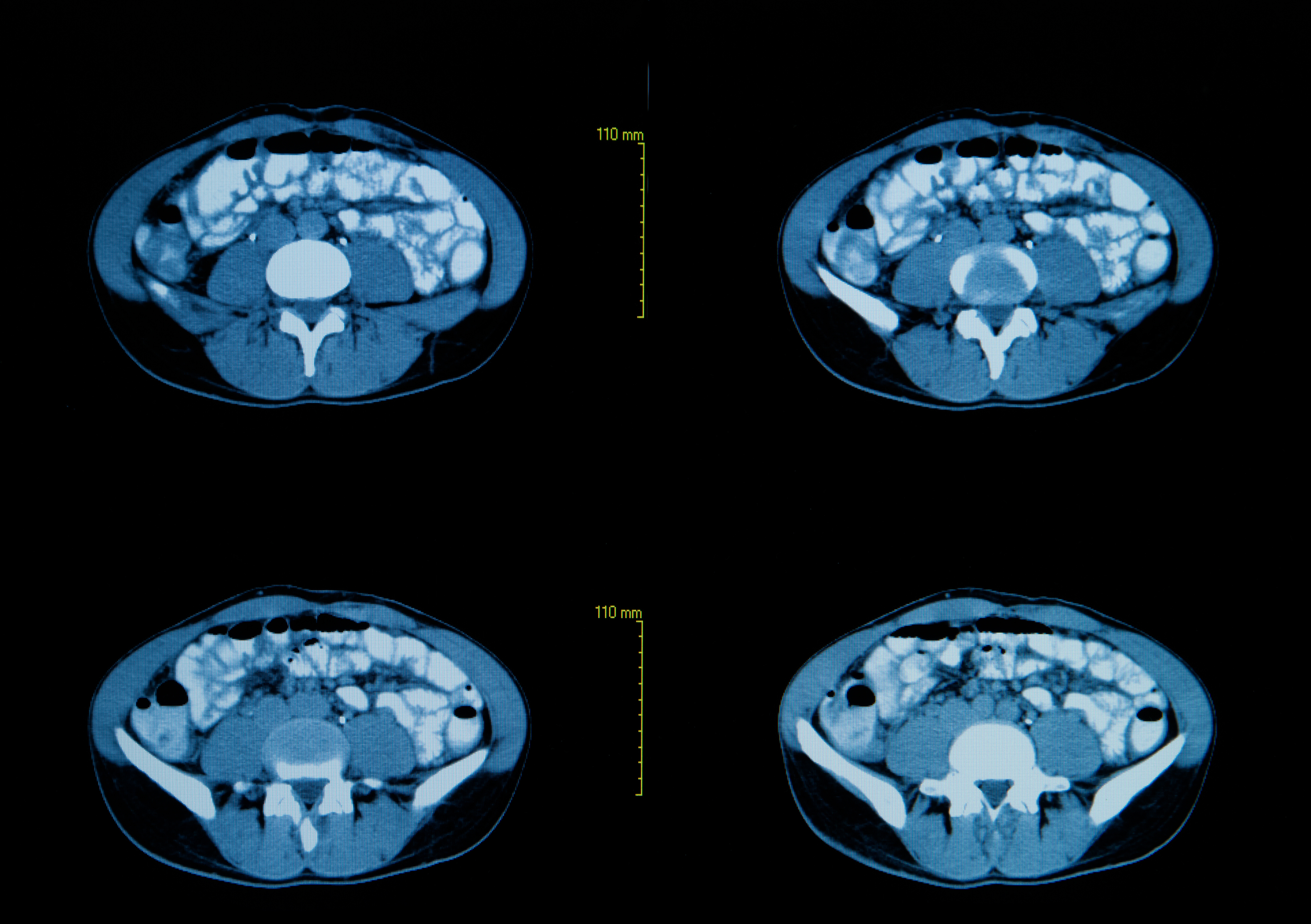
Researchers at Oslo University Hospital – Rikshospitalet and the University of Oslo in Norway recently published in the journal Arthritis & Rheumatology the finding that high-resolution computed tomography (HRCT) imaging can be used as a predictor of lung function in patients with systemic sclerosis. The study is entitled “Predictive value of serial HRCT analyses and concurrent lung function tests in systemic sclerosis.”
Systemic sclerosis, also known as scleroderma, is a rare, chronic autoimmune disease in which the body’s own immune system attacks healthy tissues resulting in a hardening and tightening of the skin and connective tissues. The disease usually affects the skin, but it can also affect internal organs such as the lungs, blood vessels and the digestive tract. Systemic sclerosis is associated with a high risk for progressive interstitial lung disease (ILD), a group of diseases that cause progressive scarring of lung tissue compromising the respiratory function and blood oxygenation.
The goal of this study was to develop a tool for individual risk stratification in terms of ILD related to systemic sclerosis. The team analyzed a cohort of 305 systemic sclerosis patients and performed serial lung fibrosis measurements, paired pulmonary function tests (PFTs) and HRCT imaging. The fibrosis extent was scored based on HRCT and represented as percentage of total lung volumes.
Researchers found that based on HRCT results at baseline, patients could be divided into three groups: I) 40 patients with more than 20% of lung fibrosis extent, II) 157 patients with 1 to 20% of lung fibrosis and III) 108 patients with no fibrosis. In a follow-up HRCT (mean of 3.1 years later) patients in group III were still found to be fibrosis free, while 11 patients from group II progressed to a lung fibrosis extent of more than 20%.
The team found that the annual fibrosis progression rate was different among the groups and that it correlated with the total forced vital capacity (FVC; the air amount that can be forcibly exhaled from the lungs after taking a deep breath). On the other hand, fibrosis progression rate was found to not correlate with the diffusing lung capacity of carbon monoxide (DLCO; the ability of the lungs to transfer gas from inhaled air to the red blood cells in pulmonary capillaries). Researchers found that baseline fibrosis extent and FVC could be predictors of an outcome of more than 20% lung fibrosis.
The team concluded that HRCT performed at baseline could be used as a predictor of fibrosis development, the rate of fibrosis progression and of a decline in pulmonary function in systemic sclerosis patients.





