Microparticles shed from cells may be linked with SSc: Study
Levels may serve as biomarkers for the disease, help predict outcomes
Levels of microparticles, tiny molecule-filled sacs shed from cells, were altered in the bloodstream of adults with systemic sclerosis (SSc), a study reports.
Elevated microparticles derived from blood-clotting platelets were associated with disease-related antibodies and longer disease duration. By contrast, lower levels of microparticles shed from endothelial cells that line blood vessels were tied to worse skin and blood vessel involvement.
These results suggest microparticles may participate in developing SSc and serve as biomarkers to predict outcomes, the researchers noted in “Microparticles: potential new contributors to the pathogenesis of systemic sclerosis?” which was published in Advances in Rheumatology.
SSc, also called scleroderma, is an autoimmune disease that may affect multiple systems in the body. It’s marked by scar tissue building up in the skin and/or several organs, such as the heart, lungs, kidney, and digestive tract.
Microparticles (MPs), or microvesicles, are tiny membrane-bound sacs shed from cells undergoing activation or apoptosis (programmed cell death), which contain cell type-specific components. Mostly shed from platelets, white blood cells, and endothelial cells, MPs have been shown to modulate inflammatory and blood clotting activities.
Studies have suggested that people with SSc have higher levels of MPs in their blood, particularly those derived from endothelial cells (EMPs) and platelets (PMPs).
Exploring relationship between microparticles, clinical disease features
Researchers in Brazil investigated the relationships between MP levels in the blood of 70 adult SSc patients and their clinical features. Nearly all were women (90%) with a mean age of 48.9 and a mean disease duration of 6.4 years. Thirty-five sex- and age-matched healthy controls were recruited as controls.
Limited skin involvement occurred in most patients (62.9%), as well as interstitial lung disease (54.3%), marked by scarring (fibrosis) of the lungs. About vascular complications, 40% showed a late scleroderma pattern (characterized by a severe loss of tiny blood vessels), 55.7% a history of digital ulcers, and 5.7% had pulmonary arterial hypertension (PAH).
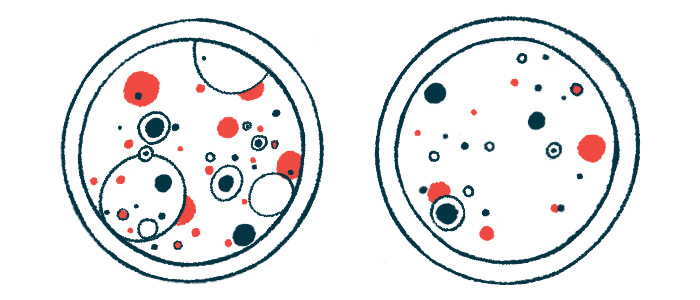
Blood tests showed SSc patients had significantly higher levels of all types of MPs compared to healthy controls, including PMPs (79.2% vs. 71%), EMPs (43.5% vs. 37.8%), and those derived from monocytes (3.5% vs. 1.1%), a type of white blood cell.
Significantly higher levels of platelet-derived MPs were found in patients who tested positive for antibodies against Scl-70, a type of scleroderma-related autoantibody, than those who tested negative (85.9% vs. 77.7%). Elevated PMPs were also found in those who had SSc for more than three years compared with those with shorter disease duration (82.4% vs. 71.6%).
The study was the “first to demonstrate increased [blood] plasma levels of PMPs in patients with SSc who were positive for anti-Scl-70 and had a longer disease duration,” the researchers wrote.
EMP levels were significantly lower in SSc patients with a modified Rodnan skin score (mRSS), a measure of skin fibrosis, of more than 15 than those up to 15 (40% vs. 44.3%). Higher mRSS reflects more severe scarring at multiple skin locations.
Low EMPs were also found in those with more severe small blood vessel loss (39.8% vs. 45%), suggesting that “might be a useful biomarker of vascular damage in SSc,” the researchers said.
MP levels were not linked to disease subtype, either limited to skin or diffuse with organ involvement, active digital ulcers, interstitial lung disease, PAH, swallowing difficulties, or heart and kidney involvement. Also, using medicines to widen blood vessels (vasodilators) or suppress immune responses didn’t affect bloodstream MP levels.
“The demonstrated association of MPs with clinical SSc features … indicates that these biologic agents may somehow contribute to the pathogenic mechanisms of this defiant disease and deserves further investigation,” the researchers said. “Our findings, along with previous studies, therefore reinforce the possible role of these molecules as prognostic [outcome] markers in SSc.”