Scleroderma Patients at Higher Risk for Developing Pulmonary Arterial Hypertension
Written by |
Patients with Systemic Sclerosis (SS), also known as scleroderma, have the highest risk of developing pulmonary arterial hypertension (PAH), according to PH expert Harrison Farber, MD who recently presented his findings at the American College of Rheumatology State-of-the-Art Clinical Symposium.
Farber presented data showing that 60% of patients with PAH are affected by some type of scleroderma, a chronic systemic autoimmune disease characterized by hardening of the skin. Registering a significantly lower risk are patients with systemic lupus erythematosus (SLE), another type of autoimmune disease, affecting 17% of patients.
As such, detecting PAH among scleroderma patients is crucial, and while the American College of Rheumatology recommends that patients undergo an echocardiogram to detect PAH, a highly sensitive diagnostic method, Farber suggests patients should ultimately be diagnosed using right heart catheterization (RHC), since its is considered the most accurate exam for measuring pulmonary artery pressures and diagnosing PAH.
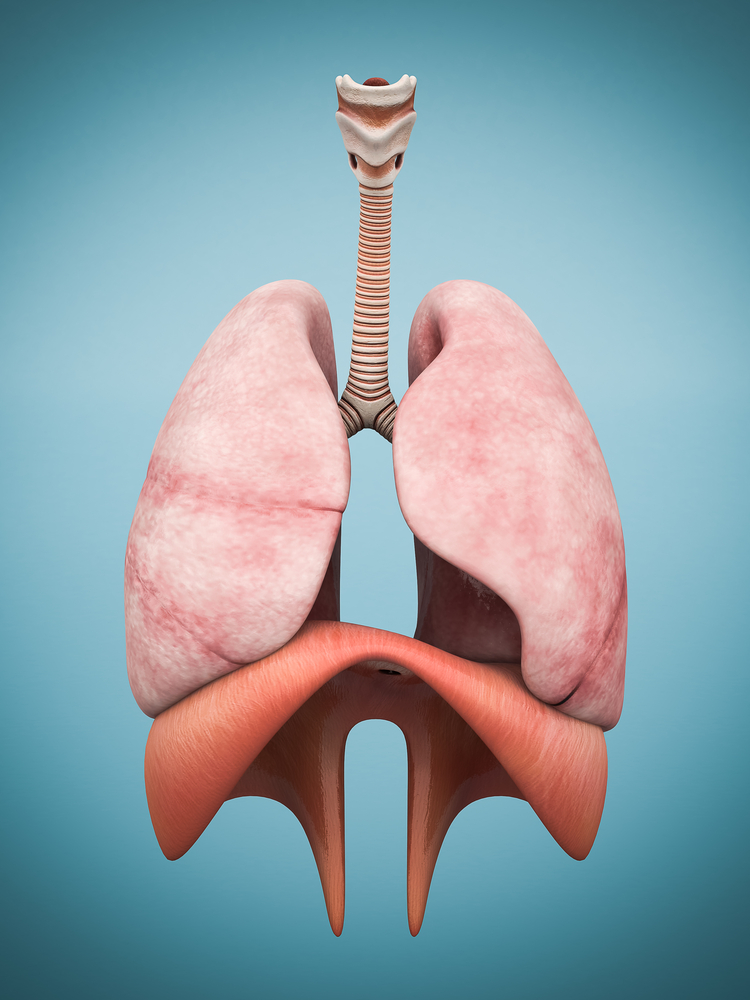
Despite scleroderma patients having higher life expectancies compared to even a few years ago, PAH and interstitial lung disease are the leading causes of death in this patient population, as Farber noted: “People with PAH and scleroderma do much worse than patients with idiopathic disease or almost any of the other subgroups. They are much more likely to die from their disease.” Other factors, such as age, pericardial effusion and liver disease are established as additional risks.
Diagnosing scleroderma patients with PAH is essential for patients to receive the best and most timely treatments, however, the diagnosis can take up to two years, according to Farber. The delay is due to patients’ frequent lack of clear symptoms, and a conclusive diagnosis is usually not made until a 6-minute walk test is used, wherein most patients with PAH score poorly.
An earlier diagnosis will allow patients to receive the proper therapy, such as prostacyclin, leading to better patient outcomes. As Farber noted, “If you look at the way [these patients] are treated, they are less frequently put on prostacyclin, which is considered the most-potent classification of drugs we can use, and … although they don’t typically respond to calcium channel blockers, typically, they are taking them.”
Results from a clinical trial with patients with PAH who received rituximab, a monoclonal antibody, and whose outcomes were compared to other standard therapies will be published later this year.





