Scleroderma Patient with Pulmonary NH Lymphoma Highlights Risk
Written by |
Researchers at St. Elizabeth’s Medical Center in Stow, Massachusetts, recently reported a clinical case of pulmonary lymphoma in a patient diagnosed with scleroderma. The data was presented at the American College of Chest Physicians Annual Meeting (CHEST 2015), held Oct. 24–28 in Montreal, Canada, under the title “Primary Pulmonary Diffuse Large B-Cell Lymphoma in Scleroderma – A Case Report” in a session on Lung Pathology Case Report Posters.
Lymphoma refers to a cancer that affects immune cells called lymphocytes, a type of white blood cell that defends the body from infections. Patients with lymphoma may experience swelling of the lymph nodes, fever, night sweats, itching, loss of appetite, sudden weight loss, and fatigue. Around 85% of all the lymphoma cases are diagnosed as non-Hodgkin’s lymphoma (NHL).
Primary NHL of the lung is a rare condition accounting for 0.4% of all lymphoma cases. However, an increased incidence has been observed in patients with scleroderma when compared to the general population. Scleroderma has also been associated with a high risk for progressive interstitial lung disease (ILD), a group of diseases that cause progressive scarring of lung tissue compromising the respiratory function and blood oxygenation.
At CHEST 2015, researchers presented a case report of an 85-year-old woman diagnosed with scleroderma and ILD, who was experiencing fever and productive cough for three weeks.
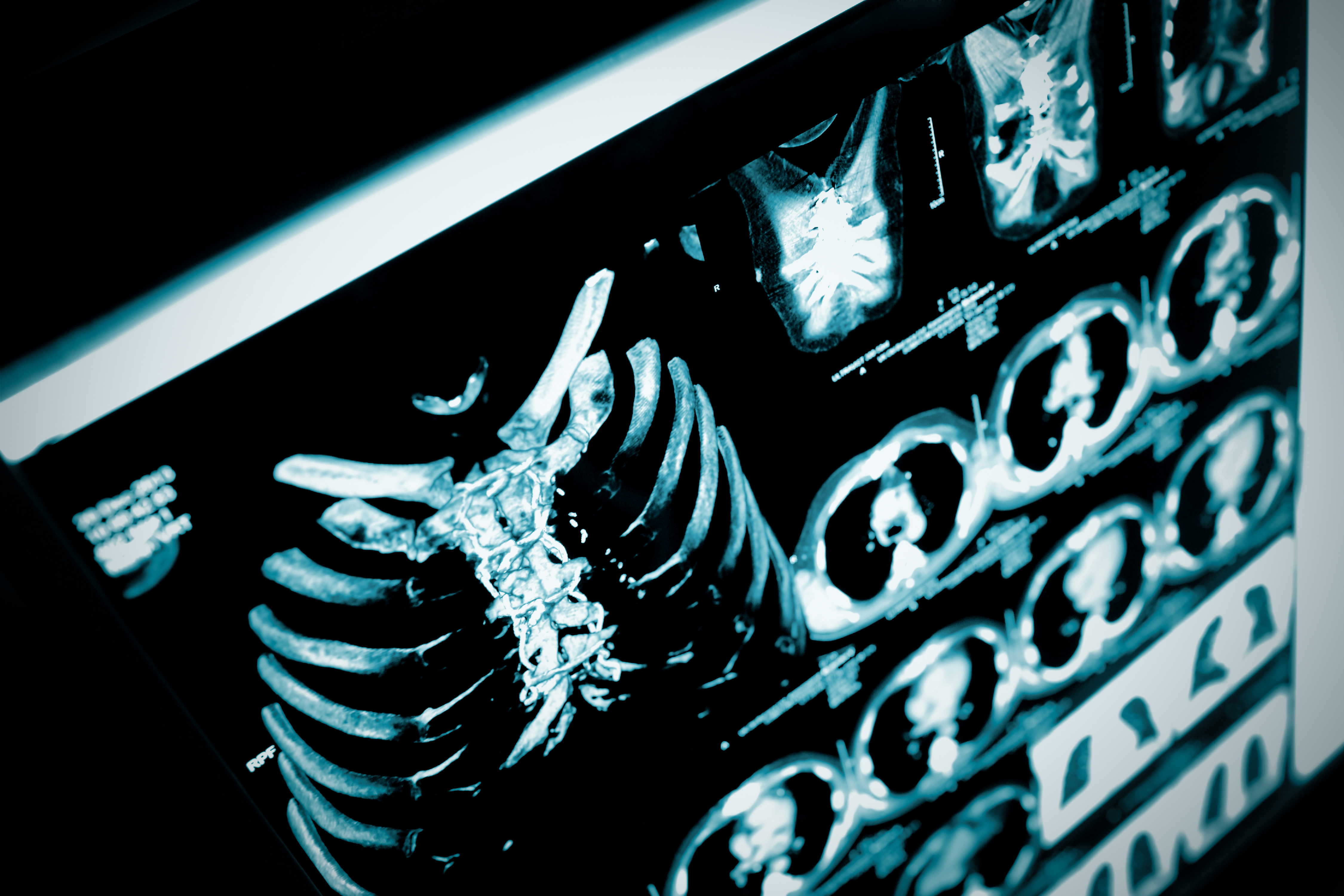
A computed tomography (CT) scan of the patient’s chest showed a right upper lobe lesion and a left lingular density. The patient’s airways were examined through a bronchoscopy procedure, and samples of the airway tested negative for bacteria or fungi. The patient received treatment with levofloxacin (a broad-spectrum antibiotic) for two weeks, but continued complaining of night sweats and dry cough.
Three months later, a new CT scan to the chest revealed almost complete resolution of the right upper lobe cavitary lesion, but enlargement of the lingular mass as well as enlargement of the mediastinal lymph nodes. Clinical examination and a CT scan of the abdomen and pelvis did not reveal any signs of extra-thoracic disease. A biopsy of the mediastinal lymph nodes was negative for malignant cells. The biopsy of the lingular mass, however, was consistent with diffuse large B-cell lymphoma (DLBCL; a condition estimated to occur in only 10% of the primary pulmonary NHL cases). At the time, the patient declined chemotherapy treatment and chose hospice care.
Researchers believe that scleroderma patients might be at increased risk for lymphoproliferative disorders due to an impaired tumor surveillance caused by defective B-cell and natural killer cell activity.
The research team emphasizes that clinicians should be aware of the increased risk for lymphoproliferative disorders, such as pulmonary NHL, when examining scleroderma patients.





