Scleroderma May Impair Ability to Eliminate Excess Cholesterol
Written by |
People with scleroderma have abnormal levels of several fatty molecules and their body’s ability to remove excess cholesterol is lower when compared with healthy peers, according to a recent study.
This impaired ability to remove excess cholesterol may contribute to an increased risk of subclinical atherosclerosis and cardiovascular diseases, but further research is needed to clarify this, researchers said.
In addition, this deficiency was significantly associated with increased skin thickness, a marker of disease severity and damage.
The study, “HDL cholesterol efflux capacity and lipid profile in patients with systemic sclerosis,” was published in the journal Arthritis Research & Therapy.
Scleroderma, also known as systemic sclerosis (SSc), is characterized by blood vessel abnormalities, increased inflammation, and tissue scarring. As the disease progresses, the skin becomes progressively thicker and internal organs increasingly scarred.
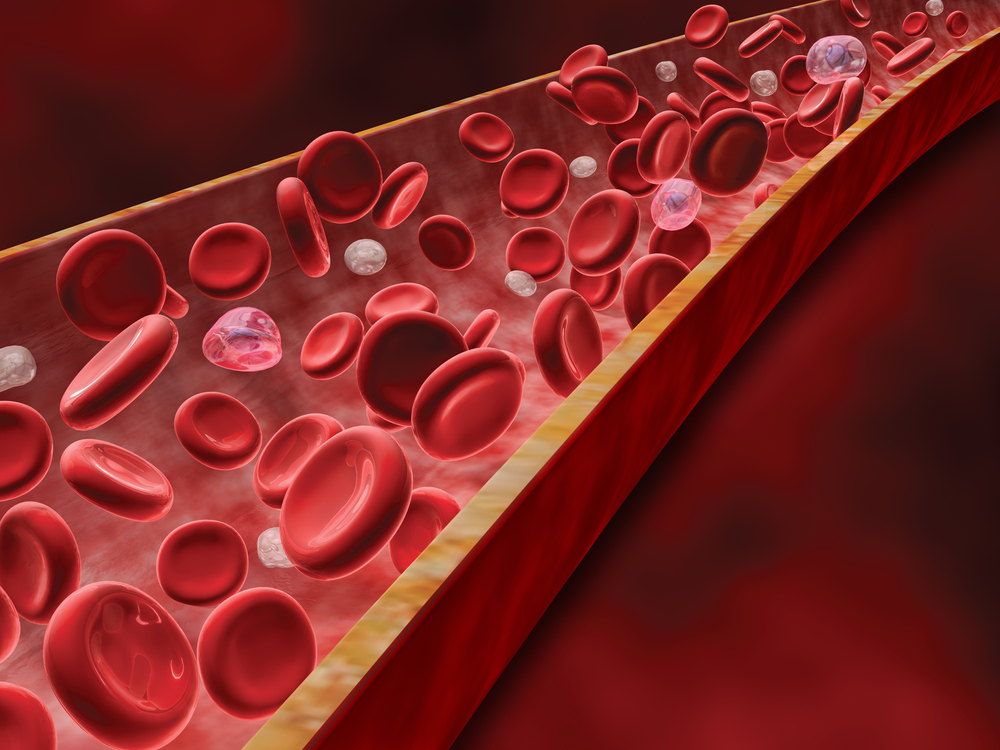
Scleroderma patients have a higher risk of subclinical atherosclerosis and cardiovascular diseases. Atherosclerosis, the leading cause of cardiovascular disease, refers to the narrowing and hardening of arteries due to the buildup of fatty deposits called plaques around the artery wall.
While the underlying mechanisms of this increased risk remain largely unclear, some studies have reported abnormal levels of fatty molecules in people with scleroderma.
However, no study has evaluated whether these patients have an impaired ability to carry excess cholesterol (a key component of plaques) from other parts of the body to the liver for removal. This transport is mediated by the high-density lipoprotein (HDL), also known as “good” cholesterol.
Cholesterol efflux capacity (CEC) is the ability of a person’s HDL to extract cholesterol from atherosclerosis-promoting immune cells, a key step of excess cholesterol removal from the body. Notably, previous studies have shown that lower CEC is associated with cardiovascular events.
In the new study, researchers in Spain evaluated the fatty molecule profile and the ability to remove excess cholesterol from the body — as assessed with CEC — in 73 adults with SSc (mean average age of 59) and 115 age- and sex-matched healthy individuals, used as controls.
They analyzed demographic information, clinical data, levels of fat-related molecules in the blood, and CEC in all participants.
Nearly two-thirds of patients had limited SSc, while about one-third had the diffuse form that is linked to more extensive skin scarring. They had been living with the disease for a mean of nine years and showed relatively mild skin thickening, as assessed with the modified Rodnan Skin Score.
No differences were found between the groups in body mass index (a measure of body fat) and the presence of high blood pressure, current smoking, diabetes, or obesity — all known risk factors of cardiovascular diseases.
However, waist circumference and current use of statins (primarily used to lower cholesterol) were significantly higher in SSc patients than in controls.
Results showed that the levels of several fat-related molecules and CEC were significantly different between the two groups.
After adjusting for waist circumference, statin use, cardiovascular risk factors, and all fat-related molecules found at different levels, SSc patients still showed significantly lower levels of total cholesterol (which includes HDL and low-density lipoprotein), and higher levels of triglycerides and lipoprotein A (also known as “bad” cholesterol).
These differences between patients and controls support the notion that systemic inflammation promotes a reduction in some fat molecules, such as total cholesterol, the team said.
Notably, CEC was significantly lower in people with SSc, compared with controls, suggesting an impaired ability to remove excess cholesterol and prevent atherosclerosis.
The team then analyzed potential associations between CEC and several demographic, clinical, and blood factors.
They found no link between traditional cardiovascular risk factors, fat-related molecules, or statin use and CEC in either group, which is consistent with data reported in previous studies.
Particularly for statins, these results support previous studies suggesting that “statins most likely confer their therapeutic benefits by means of a mechanism different from that promoting cholesterol efflux,” the team wrote.
However, more severe skin thickness was significantly associated with a lower CEC, suggesting that greater severity of SSc may further impair the ability of patients to eliminate excess cholesterol, and increase the risk of atherosclerosis and cardiovascular diseases.
“Considering this relationship between reduced CEC and [cardiovascular] risk, it is reasonable to infer that CEC reduction may contribute to the increased atherosclerotic burden suffered by SSc patients,” the researchers wrote, adding that further studies are needed to confirm this hypothesis.





