Everolimus in Fat Droplets Eased Scleroderma Symptoms in Aged Mice

The immunosuppressant everolimus, carried aboard droplets of fat (liposomes) to lung cells may ease scarring and inflammation linked to systemic scleroderma (SSc), a study with aged mice found.
The findings provide “preclinical evidence of everolimus as an efficient drug to reduce lung fibrosis [scarring] and inflammation,” its researchers wrote.
The study, “Everolimus targeted nanotherapy reduces inflammation and fibrosis in scleroderma-related interstitial lung disease (SSc-ILD) developed by PSGL-1 deficient mice,” was published in the British Journal of Pharmacology by a team of researchers in Europe.
Scleroderma is caused in part by an overactive immune system that turns against the body’s own tissues. This results in inflammation that damages the skin and can sometimes affect blood vessels and internal organs.
When lungs get damaged, their tissue stiffens and scars, making it harder to breathe. Some medications may ease inflammation but fail to work against fibrosis, and those that do work against it are often toxic.
Developed originally as a medication to slow the growth of tumors, everolimus also eases inflammation and prevents fibroblasts from dividing. A fibroblast is a connective tissue cell that makes collagen, a protein that builds up during fibrosis to form scars.
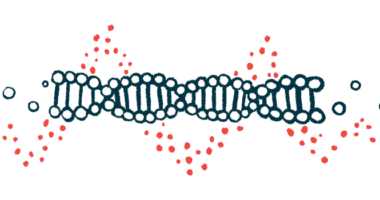
To get everolimus delivered to the lungs where it’s needed, the researchers packaged it aboard liposomes wrapped in hyaluronic acid, a molecule that acts as a cushion in connective tissue. Hyaluronic acid binds specifically to CD44, a protein receptor on the surface of cells such as fibroblasts and macrophages.
The researchers then turned to mice that develop a disease similar to the human SSc to find out how well these everolimus-containing liposomes could ease lung fibrosis and inflammation. These mice lack PSGL-1, a protein that helps recruit white blood cells into inflamed tissue. As these mice age beyond a year, most develop interstitial lung disease, a group of conditions marked by lung fibrosis.
Compared with healthy (wild-type) mice older than a year, PSGL-1-deficient mice of the same age had more CD44 in their lung cells. They also had more immune cells and myofibroblasts (a type of fibroblast able to contract) in bronchoalveolar lavage fluid samples taken from the lungs. Some of these cells made and secreted cytokines that act as “on” signals for fibrosis and inflammation.
Researchers found that the lung tissue of PSGL-1-deficient mice had more immune cells, more dying cells, and more fibrosis than wild-type mice.
For the study, the mice were either left untreated or treated with four doses of 50 microliters (mcl) of liposomes, one dose per week. The liposomes were either empty or contained everolimus at 85 mcl per mcl of solution. They were delivered using an insufflator into the trachea (windpipe) so they could reach the damaged tissue directly.
Untreated PSGL-1-deficient mice had a moderate degree of lung injury, which was maintained in treated animals, but treatment eased inflammation severity from moderate to mild.
Similar findings were obtained for lung fibrosis around the bronchi (the tubes that connect the trachea to the lungs) and in the spaces around the airways.
In line with the reduction in fibrosis and inflammation, the researchers observed that everolimus-containing liposomes reduced the number of immune cells and myofibroblasts as well as the levels of pro-fibrotic and pro-inflammatory cytokines in PSGL-1-deficient mice.
While delivery of the empty liposomes resulted in an increase in the numbers of some types of pro-inflammatory immune cells, “everolimus was clearly able to counteract the increment of inflammatory cells in lungs,” the researchers wrote.
In turn, the empty liposomes led to a decrease in certain cytokines, perhaps due to the presence of hyaluronic acid, which could have helped everolimus ease inflammation.
Together, the findings point to everolimus-containing liposomes as “a viable strategy to specifically target fibrotic lung cells,” the researchers concluded.