Proteins Linked to Scarring, Immune Cell Activation Found at High Levels in dcSSc
Written by |
Proteins involved in scarring and the escape of immune cells from blood vessels towards nearby tissues are found at high levels in people with diffuse cutaneous systemic sclerosis (dcSSc), a new study reports.
The findings also revealed that greater levels of specific proteins correlated with more severe thickening of the skin.
The study, “Large-scale characterization of systemic sclerosis serum protein profile: Comparison to peripheral blood cell transcriptome and correlations with skin/lung fibrosis,” was published in the journal Arthritis & Rheumatology.
Scleroderma, or systemic sclerosis, causes fibrosis (scarring) in multiple organs. The disorder results from the production of autoantibodies that mistakenly recognize the body’s own tissues as targets. The disease mechanisms underlying scleroderma, however, are not fully understood.
Previous research has gained insights into such processes by looking at the role of DNA and RNA, but few studies have focused on the role of proteins, particularly those found in the blood of scleroderma patients.
In this study, researchers at The University of Texas Health Science Center at Houston and their colleagues analyzed a large panel of 230 proteins in blood samples of 66 dcSSc patients (mean age 45.3 years, 60.6% women) and compared their levels to those found in 66 age- and sex-matched healthy individuals who served as controls.
The patients took part in the Phase 2/3 SCOT trial (NCT00114530), which showed that stem cell transplant confers greater benefits compared to Cytoxan (cyclophosphamide) in people with severe scleroderma.
Most patients presented autoantibodies against the cell nucleus, or antinuclear (86.4%), with nearly 40% having anti-topoisomerase antibodies. Their mean disease duration was 2.3 years.
The protein analysis showed that the levels of 90 out of 182 proteins were different between dcSSc patients and controls. Notably, 27 patients who had received immunotherapy two months before the blood sample collection showed a similar profile to the remaining participants with dcSSc.
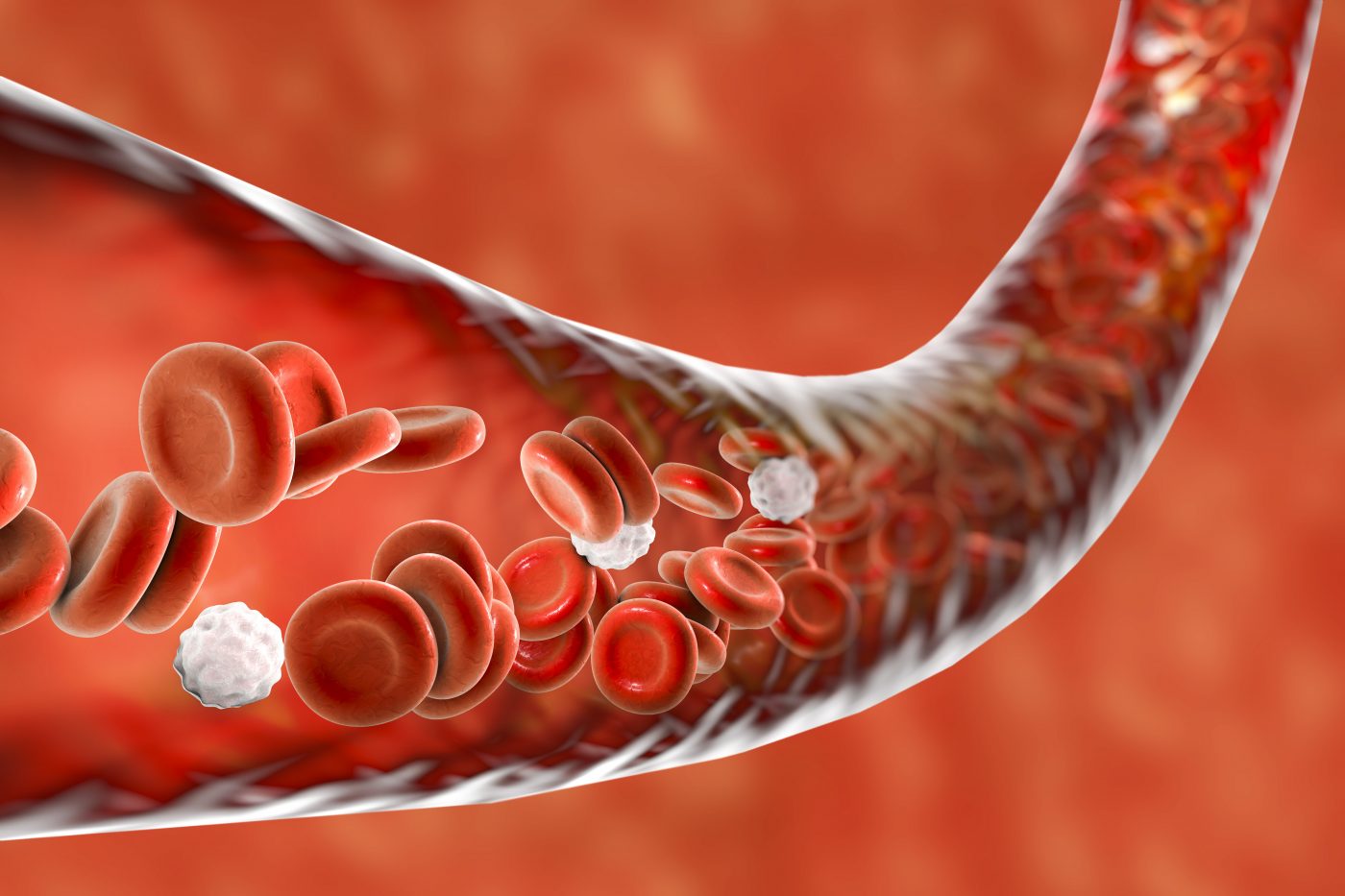
Further analysis revealed that the participants with dcSSc had higher levels of proteins linked to three main biological pathways: liver fibrosis, granulocyte adhesion and diapedesis, and agranulocyte adhesion and diapedesis.
Diapedesis is the term used to described the passage of activated immune cells from blood vessels towards a nearby tissue. Granulocytes are a type of white blood cells characterized by specific granules, with agranulocytes lacking such granules.
The researchers predicted that the top enriched cytokines — small molecules involved in immune response mediation — and growth factors in those with dcSSc were pro-fibrotic proteins, including oncostatin, interleukin (IL)-6, IL-18, and monocyte chemotactic protein 1.
Among the 90 proteins found at greater levels in dcSSc blood samples, 40 (44.4%) are linked to type I interferons, a key immune response.
Next, the scientists investigated the association of this distinct protein profile with the clinical presentation of dcSSc.
They found that alpha 1 antichymotrypsin, endostatin, osteopontin, tenascin, insulin growth factor binding protein 4, and a cardiac health marker known as NT proBNP were present at higher levels in dcSSc samples than in controls. Also, higher levels of these proteins correlated with greater skin thickness, as measured by the modified Rodnan Skin Score (mRSS).
The blood levels of NT proBNP and of the growth factor angiopoietin 2 predicted a higher level of mRSS in the future, while blood levels of epidermal growth factor receptor and kallikrein-5 predicted a subsequent lower mRSS in participants treated with Cytoxan.
Regarding lung involvement, the researchers found that two proteins — called carcinoma antigen 15.3 (CA 15.3) and growth regulated alpha protein — were associated with a lower forced vital capacity (a measure of lung function) and higher scores in the assessment of interstitial lung disease, indicative of more severe complications.
To understand the origin of these proteins, the investigators compared their levels with those of their messenger RNAs (mRNAs) in the blood. Notably, mRNAs are the molecules generated from DNA and used as the template for protein production.
The results showed that the levels of 52 mRNA molecules were significantly different in dcSSc compared to controls. Twenty-four mRNAs corresponded to a protein also produced at different levels in the two groups. However, while differences in 17 mRNAs (corresponding to 14 genes) were in agreement with those of the associated proteins, results in seven mRNA molecules showed opposite variations when comparing differences between the dcSSc and control groups, “indicating that the observed differential expression in the serum [blood] proteins does not stem from peripheral blood cells,” the researchers wrote.
Overall, “SSc serum samples showed a distinct proteomic profile in comparison to controls which includes an activation of prominent profibrotic cytokines,” they added.





