New Study Summarizes Scientific Findings Concerning Scleroderma Renal Crisis
Written by |
 In a recent study entitled “Scleroderma renal crisis,” the authors summarize the most recent findings related to scleroderma renal crisis, a serious but treatable complication of systemic sclerosis. The study was published in the journal Seminars in Arthritis and Rheumatism.
In a recent study entitled “Scleroderma renal crisis,” the authors summarize the most recent findings related to scleroderma renal crisis, a serious but treatable complication of systemic sclerosis. The study was published in the journal Seminars in Arthritis and Rheumatism.
Scleroderma (or systemic sclerosis) is an autoimmune disease characterized by skin thickening, a process known as fibrosis. Several complications associated with scleroderma are due to the fibrosis process that is actually not restricted to the skin, reaching in severe cases, internal organs such as kidneys. As a consequence, a serious complication and a medical emergency emerges, known as scleroderma renal crisis (SRC), which occurs in 5–10% of scleroderma patients. The prognosis of affected patients was significantly improved with the introduction of aggressive treatment with angiotensin-converting enzyme inhibitors, with numbers showing a 65% patient survival rate (before treatment it was less than 10%).
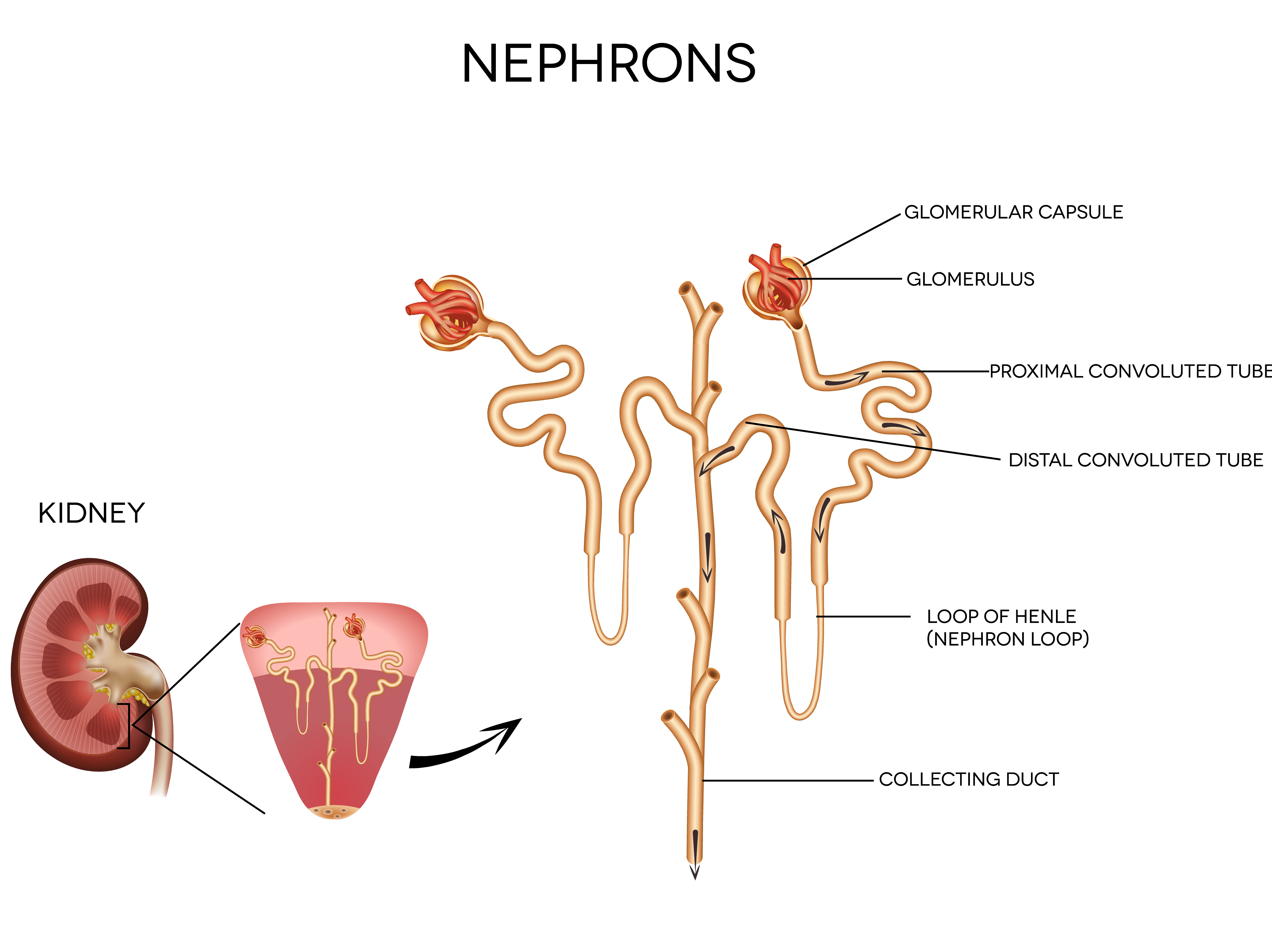
Here, the authors discussed and summarized a literature review on pathophysiology, risk factors and outcomes of SRC. The team reviewed published studies until 2013, accessible in the PubMed database, related to scleroderma and SRC. The authors were able to conclude from the meta-analyses that SRC still affects approximately 10% of all scleroderma patients and is currently described as the result of endothelial injury in the kidneys, accompanied by narrowing of kidneys arterioles (small diameter blood vessels that extend from arteries). This leads to decreased blood flow and accelerated hypertension, the latter a characteristic of SRC, together with progressive renal failure. Additionally, SRC leads to kidney hyperplasia, i.e., an increase in the number of normal cells and hyperreninemia (abnormally high concentration of renin in the blood).
[adrotate group=”3″]
In this study, the research team highlights as risk factors rapid skin thickening as well as anemia and thrombocytopenia (low blood platelet count); certain types of medications, including corticosteroids or cyclosporine and cardiac complications, such as congestive heart failure and arrhythmias are risk factors for SRC. Other factors noted in the literature also included large joint contractions and anti-RNA Polymerase III antibody — this is a specific marker for systemic sclerosis and usually associated with severe states of disease where internal organs are affected.
In terms of mortality, the authors acknowledge that with the introduction of angiotensin converting enzyme (ACE) inhibitors, mortality decreased from 76% to less than 10%. The advent of renal transplantation was also noted as a significant measure for the decrease in mortality; however, SRC can still relapse in transplanted kidneys.
The authors highlight that, despite a significant improvement obtained in recent years, SRC is still affecting a meaningful population of patients with systemic sclerosis and so a vigilant diagnosis and therapy is needed to prevent adverse outcomes and enhance survival.





