New Data Supports Moving Anti-CCL24 Therapy Into Clinical Development for SSc

New data from patient samples and a mouse model provide support for the further development of Chemomab Therapeutics‘ lead candidate, CM-101 — an antibody targeting the CCL24 protein — for the treatment of systemic sclerosis (SSc), according to two recent scientific presentations.
Encouraged by the new data, the company expects to launch a Phase 2 clinical trial of CM-101 in patients later this year.
“The growing body of data demonstrating the role of CCL24 in the pathophysiology [underlying disease mechanisms] of systemic sclerosis further supports our plans to assess our CCL24 neutralizing antibody, CM-101, as a potential therapy for systemic sclerosis in a Phase 2 trial we intend to initiate later this year,” Adi Mor, PhD, Chemomab’s chief scientific officer, said in a press release.
Mor gave a presentation, “Blocking CCL24, a novel target regulating inflammation fibrosis and endothelial damage, shows promising potential as treatment for Systemic Sclerosis” on March 7 at the International Rheumatology Conference in Israel.
The data showed that CCL24 is expressed at higher levels in the skin and blood of SSc patients than healthy individuals. Higher CCL24 levels were correlated with biomarkers of fibrosis (scarring) and disease progression.
In a mouse model of SSc, CM-101 was able to significantly reduce levels of skin and lung fibrosis when treated either before symptom onset or during active disease.
Francesco Del Galdo, MD, PhD, a University of Leeds professor, presented, “CCL24 as a Marker of Worse Prognosis in diffuse cutaneous SSc: a Promising Novel Biological Target,” on March 12 at the 7th Systemic Sclerosis World Congress.
Like Mor’s presentation, Del Galdo showed that blood CCL24 levels were associated with disease activity and progression in people with a diffuse form of SSc. In these patients, elevated CCL24 blood levels correlated with greater lung fibrosis and deterioration over time, altogether indicating a worse prognosis.
“This translational study is the first to demonstrate that high CCL24 levels in patients with diffuse cutaneous systemic sclerosis are correlated with disease activity and a worse prognosis,” Del Galdo said. “The study data supports the role of CCL24 as a potential therapeutic target for diffuse cutaneous SSc, and we look forward to an upcoming Phase 2 clinical trial assessing CM-101, a CCL24 neutralizing antibody, in systemic sclerosis patients.”
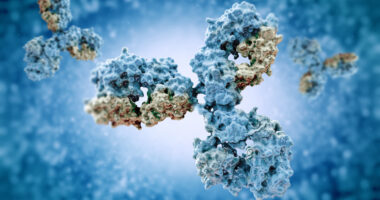
CCL24 is a type of chemokine, proteins which serve as chemical attractants to immune cells, helping to orchestrate their movement during an immune response.
Chemokines have been suggested to be involved in multiple processes critical to scleroderma development, including collagen accumulation, which is involved in fibrosis, the activation of inflammatory cells, and impairment of blood vessel formation.
Some evidence also suggests that chemokines are involved in the transition of fibroblasts to myofibroblasts — the cells responsible for the synthesis and buildup of scar tissue.
Previous data from Chemomab showed that CM-101 safely and effectively blocked CCL24, leading to reduced fibrosis in a mouse model and decreased myofibroblast formation in blood samples from SSc patients.
Chemomab and Del Gado are currently collaborating to further understand the role of CCL24 in causing blood vessel damage in SSc patients.