Systemic Sclerosis 2016 Congress Presentation Argues That Peptide May Predict Mortality Risk in SSc Patients
Written by |
At the 4th Systemic Sclerosis World Congress, recently held in Lisbon, Portugal, an international team of researchers led by Dr. Yannick Allanore from the Department of Rheumatology A, Paris Descartes University, in France, suggested a valuable predictor of mortality in patients with systemic sclerosis (SSc). The presentation was titled “N-Terminal Pro Brain Natriuretic Peptide is a Strong Predictor of Mortality in Systemic Sclerosis”(abstract C0-15).
SSc is an autoimmune connective tissue disease characterized by thickening of the skin, and caused by the accumulation of collagen and by injuries to the smallest arteries. There are two SSc overlapping forms: limited cutaneous SSc, which is limited to the skin on the face, hands and feet; and diffuse cutaneous SSc, which covers more of the skin, and is at risk of progressing to visceral organs, including the kidneys, heart, lungs, and gastrointestinal tract.
SSc patients have a poor prognosis, and while for some patients the disease remains in a stable mild form, others experience serious clinical outcomes. Cardiovascular involvement is a widely known contributor to mortality in patients with SSc.
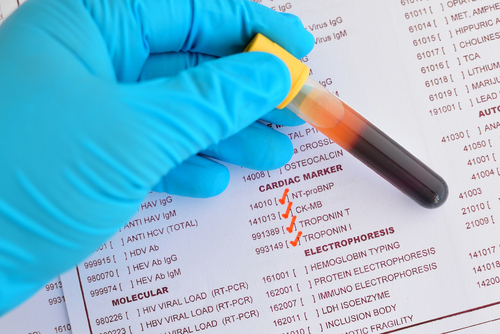
Dr. Allanore and colleagues used a cardiac biomarker known as N-terminal of the prohormone brain natriuretic peptide (NP-proBNP) to assess its accuracy as a predictor of prognostic outcomes in 523 patients with SSc (mean disease duration of 8 years, and a diffuse cutaneous form in 168 patients).
The NT-proBNP is a 76 amino acid N-terminal inactive protein that is cleaved from proBNP to release brain natriuretic peptide. NT-proBNP levels in the blood are used for the screening and diagnosis of acute congestive heart failure (CHF), and may be useful to establish prognosis in heart failure, as it is typically found in higher levels in patients with worse outcomes.
In the study, researchers measured the levels of NT-proBNP at baseline, and all patients had yearly follow-ups for five years.
Dr. Allanore reported that at baseline, 37 SSc patients had cardiovascular involvement (17 had pulmonary arterial hypertension and 20 had reduced left ventricular ejection fraction). In total, 32 patients died within three years, and 59 within five years. Importantly, results revealed that NT-proBNP was elevated in those patients who died within three years, and within five years, compared to those who survived all follow-up examinations.
Based on the results, researchers concluded that NT-proBNP, at a cutoff value of 125 ng/L, was strongly and independently associated with three- and five-year mortality in SSc patients, representing a potential predictor of mortality in this patient population.





