Lung Blood Vessel Disease in Systemic Sclerosis May Be Caused by Endothelial to Mesenchymal Cell Switch
 Researchers at the Centre for Rheumatology and Connective Tissue Disease at University College London have found new evidence that could help in understanding how lung blood vessel disease (pulmonary vasculopathy) in systemic sclerosis develops. The study could form the basis for future treatments that block the condition from occurring. The work was presented at the recent American College of Rheumatology Meeting, held from November 14-19 in Boston, Massachusetts.
Researchers at the Centre for Rheumatology and Connective Tissue Disease at University College London have found new evidence that could help in understanding how lung blood vessel disease (pulmonary vasculopathy) in systemic sclerosis develops. The study could form the basis for future treatments that block the condition from occurring. The work was presented at the recent American College of Rheumatology Meeting, held from November 14-19 in Boston, Massachusetts.
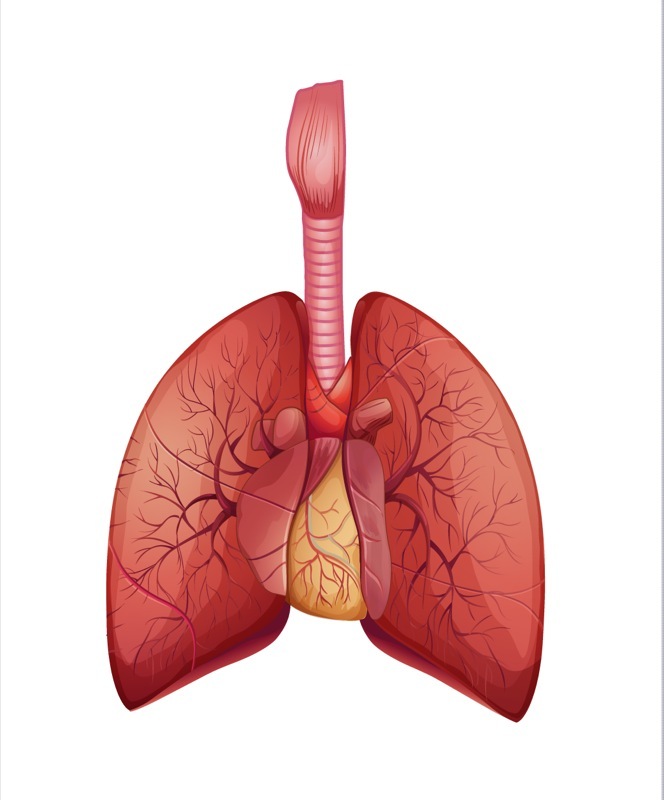
Vasculopathy in systemic sclerosis is associated with a high risk of death, especially in people who develop pulmonary arterial hypertension (SSc-PAH). Pulmonary vasculopathy may occur because the endothelium — a single layer of cells lining blood vessels — has transformed to a pathological state. This state is called an endothelial-mesenchymal transition (EndoMT), meaning the endothelial cells have actually turned into a different cell type, the mesenchymal cell. Mesenchymal cells are “undifferentiated,” so they do not have specific cell characteristics. EndoMT causes several problems, including blood leak and inflammation, perhaps because the mesenchymal cells are in an indeterminate state — one that is not functional or protective in the lungs.
Focusing on the endothelial cells and how they transform to a diseased mesenchymal state may be particularly important for understanding pulmonary vasculopathy in systemic sclerosis and for developing treatments for this condition.
Lead author Dr. Robert Good and his colleagues took lung tissue from three people with SSc-PAH and compared it to tissue donated by three people without lung disease. The investigators also studied a mouse model in which lung disease had been induced. They used various measurements of cellular activity to see what characteristics occur when cells undergo EndoMT. They identified EndoMT based on previously established criteria: markers called vWF and αSMA that were measured using a fluorescent dye.
The investigators found the markers for the EndoMT in about 5% of the blood vessels from the people with SSc-PAH and the lung-diseased mice. They further found that cells undergoing EndoMT secrete several inflammatory molecules known as cytokines, including interleukin-6 (IL-6). When they treated healthy lung cells with inflammatory cytokines they were able to induce EndoMT: cell markers for endothelial cells disappeared and were replaced by markers for mesenchymal cells. They further found that EndoMT cells failed to form a normal cellular barrier in the lungs, possibly contributing to increased vulnerability to toxins or other insults.
In their presentation, the researchers concluded “Collectively our data suggests that EndoMT may contribute to the loss of normal endothelium function and the development of SSc-PAH.” Future studies may focus on ways to prevent EndoMT from occurring, possibly by blocking some of the inflammatory molecules identified in this study.






