Key Antibodies Present in Scleroderma, Systemic Lupus Erythematosus
Written by |
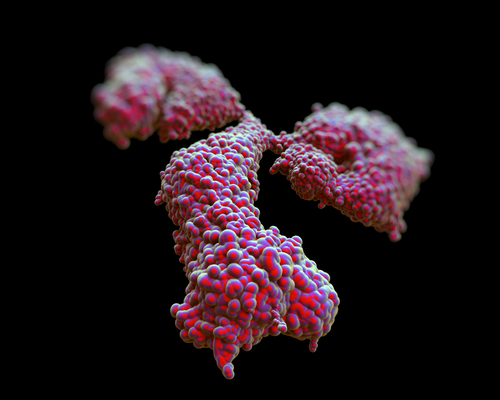
 A new study entitled “Increased frequency of class I and II anti-human leukocyte antigen antibodies in systemic lupus erythematosus and scleroderma and associated factors: a comparative study” published in October issue of the International Journal of Rheumatic Diseases reports increased levels of anti-HLA antibodies in the autoimmune disorders systemic lupus erythematosus (SLE) and scleroderma (SSc).
A new study entitled “Increased frequency of class I and II anti-human leukocyte antigen antibodies in systemic lupus erythematosus and scleroderma and associated factors: a comparative study” published in October issue of the International Journal of Rheumatic Diseases reports increased levels of anti-HLA antibodies in the autoimmune disorders systemic lupus erythematosus (SLE) and scleroderma (SSc).
Systemic lupus erythematosus and scleroderma (SSc) are two types of autoimmune diseases — disorders where there is an abnormal immune response against the body itself. Both disorders were previously associated with increased production of autoantibodies (which means produced against an individuals’ own proteins). In this study, the authors measured the levels of anti-human leukocyte antigen (HLA) antibodies, the major cause of organ transplant rejection and associated also with autoimmune diseases. The study was conducted among 77 patients with SLE, 46 patients with SSc, and 53 healthy patients who served as controls for the study. The data was collected through the use of hospital records. In order to conduct an anti-human leukocyte (anti-HLA) antigen antibody analysis of sera, Lifecodes anti-HLA Class I and Class II Screening kits based on xMAP technology were used.
In both SLE and SSc patients, there was increased production of both class, I and II anti-HLA antibodies. While in SLE patients, the elevated levels were associated with secondary symptoms, in the SSc group, no association was found. Specifically, frequencies of both class I and II anti-HLA antibodies were found to be significantly higher in patients with SLE (27.3% and 41.6%) and SSc (26.1% and 41.3%), as compared to the patients studied as healthy controls (1.9% and 5.7%) (all P < 0.001). Moreoever, thrombocytopenia frequencies (P = 0.021), anti-ribonucleoprotein frequencies (P = 0.037) and anti-Ro frequencies (P = 0.027) were also all found to be significantly elevated in the class I antibody-positive SLE group. Researchers noted, however, that pericarditis was found to be less frequent (P = 0.05), and the class II antibody-positive SLE group had more frequent anti-ribosomal P antibody (P = 0.038), but less frequent active disease (P = 0.038). Finally, in the SSc group, class I antibody-positive patients had more frequent digital ulcers (P = 0.048) and anti-centromere antibodies (P = 0.01). There was no association of anti-HLA antibodies with pulmonary hypertension and interstitial fibrosis in SSc patients.
These new insights into the presence and frequency of antibodies in both SLE and SSc may lead to improved diagnostic and therapeutic options for both diseases.





