Immune Cell Tilt Toward Inflammation Seen in Aging May Fuel Scleroderma, Study Says
As people age they accumulate a subset of more pro-inflammatory monocytes, a type of immune cell, that may ultimately contribute to the persistent low levels of chronic inflammation seen in the elderly, a new study reports.
These findings may help in further understanding the mechanisms underlying inflammatory diseases, including systemic sclerosis, which is characterized by a buildup of these pro-inflammatory monocytes.
The study, “The pro-inflammatory phenotype of the human non-classical monocyte subset is attributed to senescence,” was published in the journal Cell Death & Disease.
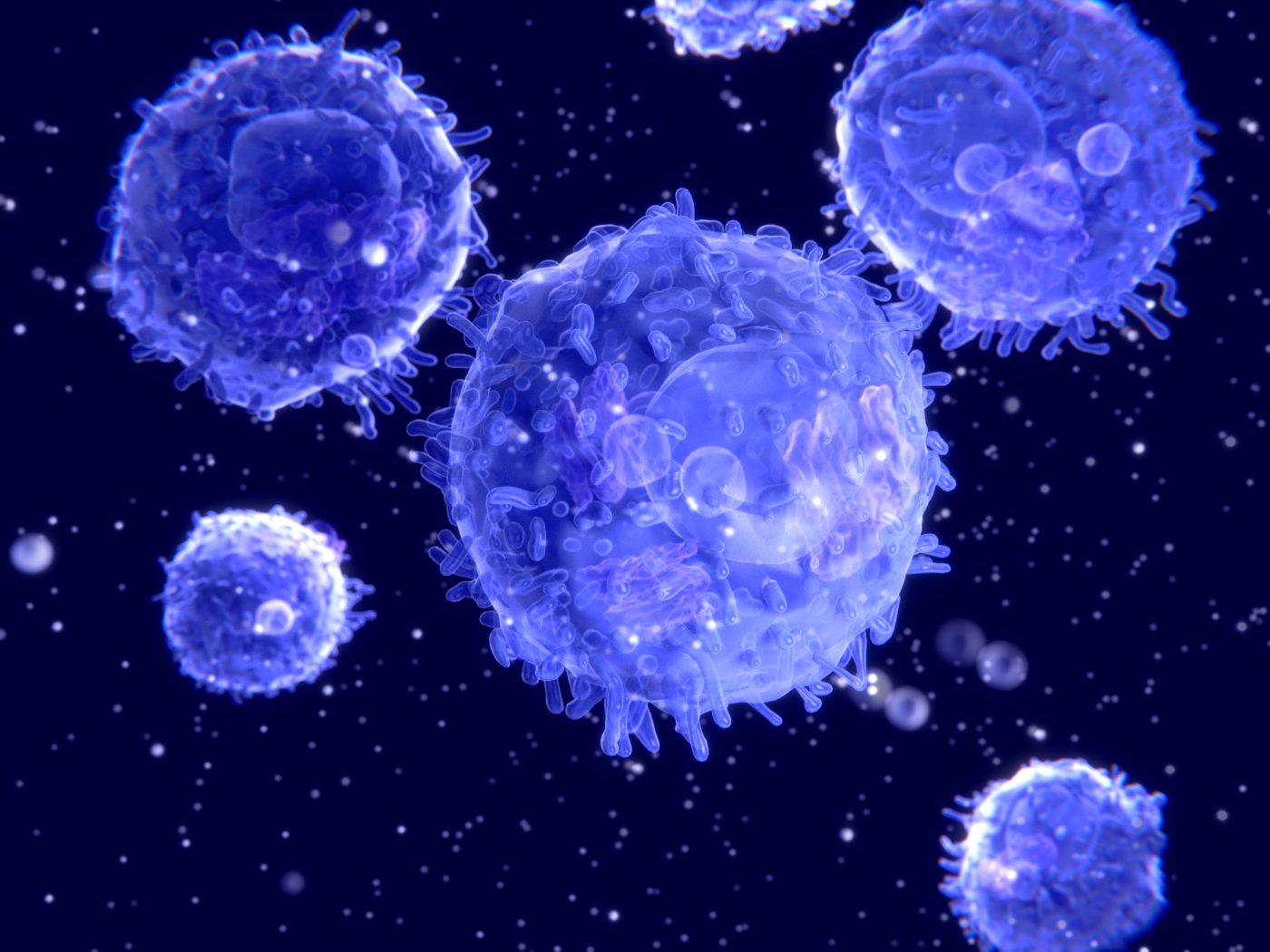
Monocytes are a type of immune cell — they belong to white blood cell group — important in the defense against pathogens, like bacteria or viruses.
A heterogenous group of cells, monocytes can be divided in three subgroups according to expression levels of two proteins, called CD14 and CD16 — classical, intermediate, and non-classical. Non-classical monocytes are the most inflammatory of the three, yet they have very high levels of a small RNA molecule, called microRNA-146a, that usually suppresses inflammatory responses.
This co-ocurrence of a pro-inflammatory status and a high miR-146a level has been associated with cellular senescence (cellular arrest; when cells stop dividing and proliferating) in other cell types.
“When the microRNA-146a level increases in cells, it acts to reduce inflammatory response in these cells,” Siew-Min Ong, a researcher at the A*STAR Singapore Immunology Network (SIgN) and the study’s first author, said in a press release.
“But what we found in the non-classical monocyte subset is the opposite — they are more inflammatory despite having a higher level of microRNA-146a compared to the other two monocyte subsets,” Ong added.
In other cell types, the presence of pro-inflammatory status and high levels of microRNA-146a has been linked with cellular senescence — cells no longer able to proliferate, and the reason senescence is associated with aging.
Researchers investigated whether the non-classical monocytes expressing high levels of the microRNA-146a were actually aging.
They looked for evidence of other markers of senescence besides arrested proliferation, including a shortening of telomeres (a cell’s internal clock), levels of reactive oxygen species (ROS), and changes in mitochondria (the cell’s energy source).
The team confirmed that among the three subsets, non-classical monocytes were the least proliferative and most senescent subset — researchers found ROS levels in non-classical monocytes double that to the classical subset, and signs of mitochondria dysfunction that further confirmed their senescent status.
Non-classical monocytes also showed a pattern of release of pro-inflammatory factors, including growth factors and signaling molecules (cytokines).
Senescent cells accumulate with age, and are considered a key contributor in the chronic, low-level systemic inflammation observed in the elderly.
Researchers then analyzed monocyte blood levels in 30 healthy, young volunteers (ages 22 to 35), and 30 healthy, elderly volunteers (55 and older).
Elderly people, compared to the younger group, had higher levels of all three subset of monocytes in their blood, but particularly in the more senescent, non-classical subset. The elderly group also had significantly higher levels of pro-inflammatory cytokines, such as tumor necrosis factor (TNF)-alpha and interleukin (IL)-8.
“With an increase in the numbers of non-classical monocytes in the elderly, we believe that their persistent low level of inflammation may be in part contributed by these cells,” Ong said.
Systemic sclerosis patients also have higher numbers of these inflammatory senescent monocytes, supporting their potential role in disease onset and progression.
“Currently, we are unclear if this is a cause or effect,” Ong said. “Either the disease makes the monocytes senesce faster and therefore we have more senescent monocytes, or the monocytes react by senescing so that they have more pro-inflammatory monocytes to fight the disease.”
Understanding why these non-classical monocytes accumulate in systemic sclerosis and other inflammatory diseases may aid in developing new ways of treating these ills.