SSc associated with worse outcomes in hospitalized COVID-19 patients
Risk was assessed by a composite score that combined several clinical measures
Written by |
Hospitalized patients with COVID-19 are more likely to have worse outcomes if they also have systemic sclerosis (SSc), a study finds.
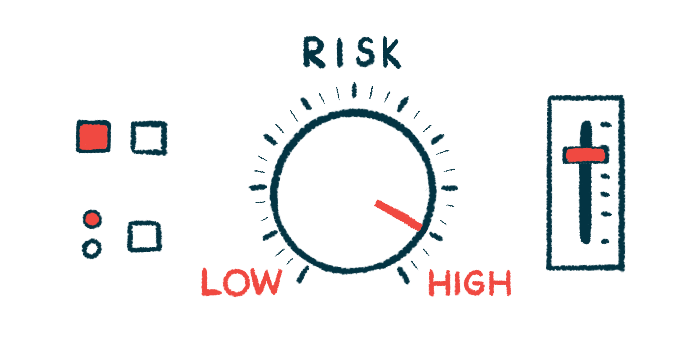
This risk was assessed by a composite score that combined several clinical measures, including in-hospital mortality, invasive mechanical ventilation to help with breathing, use of medications to raise blood pressure, acute kidney injury, and cardiac arrest. When analyzed individually, the variables didn’t show any differences between the two groups, however.
“Further studies are needed to establish a better understanding of the relationship between COVID-19 and SSc, particularly in terms of risk factors, complications, and outcomes,” the researchers wrote in “Outcomes in systemic sclerosis patients hospitalized with COVID-19: Insight from the National Inpatient Sample,” which was published in the Journal of Scleroderma and Related Disorders.
Also called scleroderma, SSc features scarring in the skin due to the excessive production of collagen, the main protein component of scar tissue. Scarring can also occur in internal organs, including the lungs, heart, kidney, and digestive tract.
People with SSc have a higher prevalence of infections than the general population, including lung infections like pneumonia. This suggests lung fibrosis may be a predisposing factor for pulmonary infections and may be associated with worse outcomes.
Both COVID-19 and SSc have an underlying autoimmune disturbance wherein the immune system mistakenly attacks the body’s own tissues, according to the researchers, so both diseases coexisting may contribute to worse outcomes from COVID-19.
Outcomes of SSc patients hospitalized for COVID-19
However, “the outcomes of SSc patients hospitalized with COVID-19 have not been well characterized,” wrote the researchers, who analyzed adults admitted to the hospital with a principal diagnosis of COVID-19 who were included in the National Inpatient Sample database from 2020. The goal was to analyze the impact of SSc on clinical outcomes and resource utilization of COVID-19 patients.
Of a total of 1,050,040 adults with a COVID-19 diagnosis, 775 (0.07%) had a secondary SSc diagnosis. These patients had a higher Elixhauser Comorbidity Index, a measure of the burden of coexisting disorders.
The proportion of women was significantly higher in the SSc group than in those without SSc (77.4% vs. 47.2%). Both peripheral vascular disease (8.4% vs 4.5%) — reduced blood circulation to a part of the body other than the heart and brain — and heart valve disease (7.1 vs. 3.9%) were also significantly more frequent in the SSc group. So were anemia (6.4% vs. 3.43%), a disorder that affects red blood cells, and underactive thyroid , or hypothyroidism (21.9% vs. 13.9%).
Those with both COVID-19 and SSc had a significantly lower prevalence of obesity (16.1% vs. 27.4%), diabetes (27.7 vs. 40.8%), and prior permanent use of implantable devices to treat heart conditions (0.6 vs. 3.6), however. SSc patients with COVID-19 did have a higher burden of interstitial lung disease — a group of diseases that feature lung inflammation and fibrosis — than those without COVID-19 (17.4% vs. 1.13%).
Although there were no statistically significant differences regarding individual disease outcomes, some measures were higher in people with SSc and COVID-19 compared to those without SSc. These included in-hospital mortality, use of medications to increase blood pressure, cardiac arrest, acute kidney injury, and requiring a visit to a health facility.
There were no differences between the two groups in the length of a hospital stay and hospital costs. The data indicate that worse outcomes with COVID-19 don’t lead to an increased healthcare burden, according to the researchers, who said more studies are needed.
The composite endpoint of major adverse events — which combines all clinical outcomes — was higher in participants with COVID-19 and SSc than in those without SSc, however. Specifically, COVID-19 patients with SSc were 1.52 times more likely to have adverse outcomes.
“This should be interpreted with caution as the individual outcomes did not differ significantly between the two groups,”wrote the researchers, who said the unknown vaccination status of participants was a limitation of the study. Also, “despite including a large total sample size, only 0.07% of the patients in this study had SSc,” said the researchers, who noted their results may be “underpowered to detect any significant differences between SSc patients and non-SSc patients with COVID-19 in … individual outcomes.”