At-risk SSc Patients Can Be Identified Using NVC, a Non-Invasive Imaging Technique
Written by |
A new technique called nailfold videocapillaroscopy (NVC) is a potential way of identifying systemic sclerosis patients at risk of disease progression and severity, according to a presentation titled “Sensitivity to Change of NAilfold Videocapillaparoscopy and Relationship with Disease Progression,” presented at the 4th Systemic Sclerosis World Congress recently held in Lisbon, Portugal.
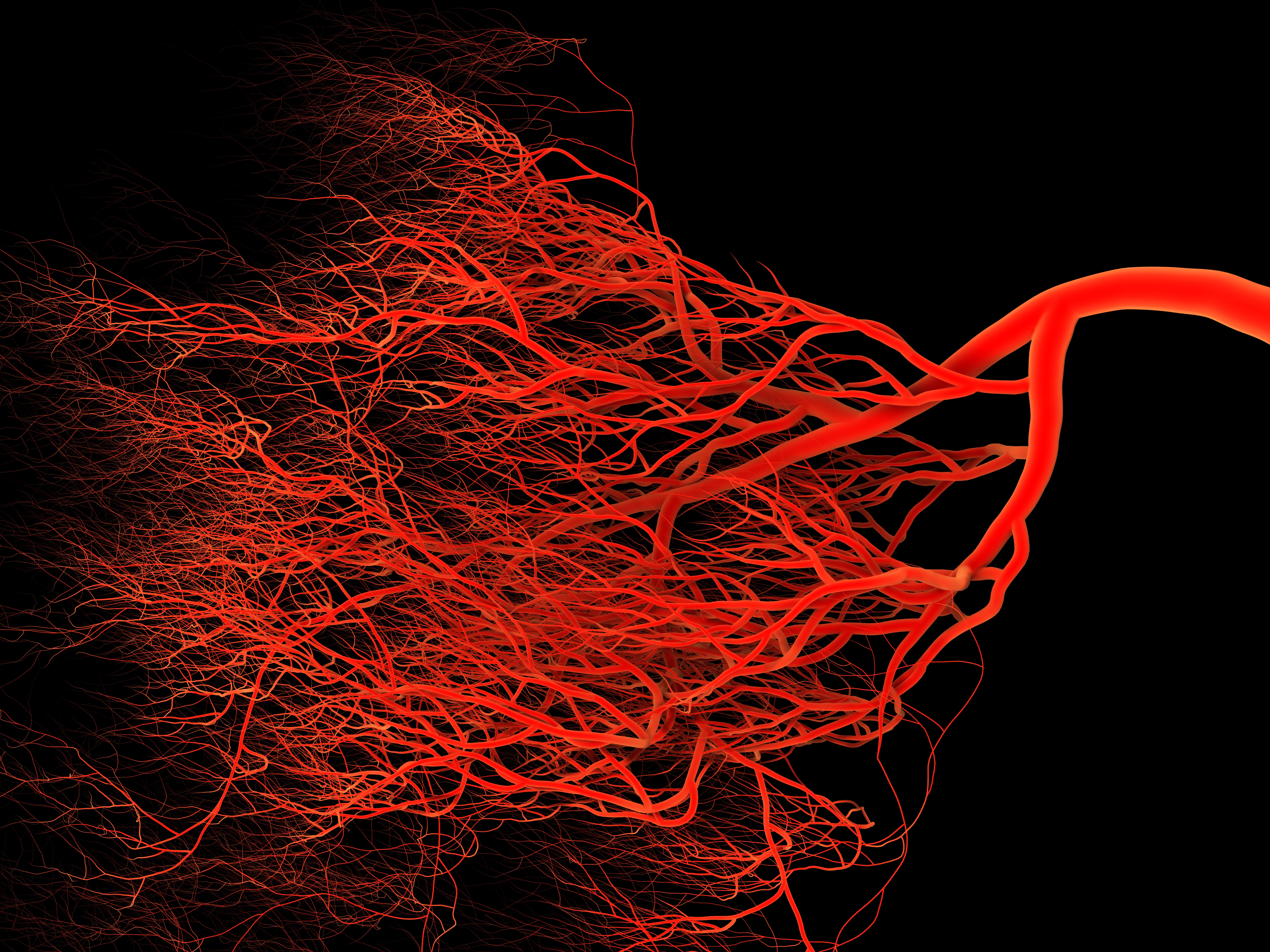
NVC is a non-invasive and inexpensive imaging technique that allows determining, with detail, skin microcirculation. It was previously reported that NVC is effective at assessing microvascular damage due to systemic sclerosis, an autoimmune disease characterized by diffuse fibrosis, degenerative changes, and vascular abnormalities in the skin and joints, but that may also affect internal organs, especially the esophagus, lower gastrointestinal tract, lungs, heart, and kidneys.
It is still not clear, however, whether NVC can detect alterations and abnormalities in the skin vascular system, and if these changes correlate with disease progression.
To this end, researchers analyzed a prospective cohort of 140 patients with systemic sclerosis, and followed them for up to three years. The NVC procedure was performed by four experienced investigators at recruitment and repeated once a year. Results were analyzed and classified as early, active, and late patterns. Disease progression was established according to the Medsger severity scale (from category 1-2 to category 3-4), and organ progression was defined according to validated definitions.
Progression from a normal/early NVC pattern to an active pattern was observed in 10 percent of participants, and patients with an active NVC pattern were more likely to have shorter disease duration (six years versus 11 years). Moreover, patients developing an active NVC pattern exhibited a significantly reduced risk for ischemic digital ulcers during follow-up. Disease progression was independent of several factors, namely age, gender, cutaneous subset, past or current digital ulcers, and use of vasodilators at baseline.
Progression to a late NVC pattern was also found in 10 percent of the screened cohort population (patients with diffuse cutaneous subset and with pre-capillary pulmonary arterial hypertension at baseline). Progression to late NVC was also independent of age, sex, disease duration, digital ulcers, and use of vasodilators at baseline. Progression was, however, associated with the occurrence of new ischemic digital ulcers, progressive lung vascular problems and skin fibrosis, as well as worsening along the Medsger disease severity scale.
In conclusion, the results supported the use of NVC as a routine strategy to evaluate patients with systemic sclerosis and to identify those at higher risks of disease progression and severity.





