Fewer Than 1 in 5 Scleroderma Patients Use Mental Health Services
Fewer than one in five scleroderma patients seek help from mental health services, an international study found.
The patients most often turned to general practitioners as their providers of mental health care, followed by psychologists and psychiatrists.
The study, “Mental health care use and associated factors in systemic sclerosis: A scleroderma patient-centered intervention network cohort study,” was published in ACR Open Rheumatology by a team of researchers at the Scleroderma Patient-Centered Intervention Network (SPIN).
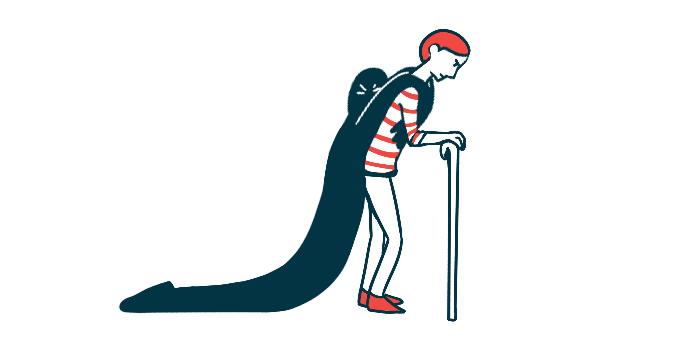
Significant psychosocial issues and emotional distress are common among people with scleroderma, also known as systemic sclerosis (SSc). Factors linked with more depressive symptoms and psychosocial impact include active and more severe disease, lung dysfunction, and skin involvement. Having lower education and not being married have also been associated with greater psychological distress among patients.
The researchers wanted to know how many patients with scleroderma seek help from mental health services. They drew on data from the SPIN cohort, a group of patients with scleroderma from seven different countries around the globe who take part in online studies.
Upon entry to the group, the patients were asked if they had visited any professional for mental health care, what type of professional, and how many times in the previous three months.
A total of 2,319 patients were included in the analysis. Many (36%) were from the U.S., 25% were from France, 24% from Canada, 11% from the U.K., and the remaining were from Spain, Australia, or Mexico. Their mean age was 54.6 years, and the majority (88%) were women.
Most (98%) experienced Raynaud’s phenomenon, which occurs when the fingers and toes feel numb and prickly under cold or stress. Other common symptoms were esophageal dysfunction (85%) and sclerodactyly (81%), during which the fingers and toes thicken and harden. Also, 40% had diffuse scleroderma, a form of SSc marked by extensive scarring over large areas of the skin and damage to the body’s internal organs.
Of the 2,319 patients, 417 (18%) said they sought help from mental health services in the three months before enrolling in SPIN.
General practitioners were the most common providers of mental health care (59%) in all countries, followed by psychologists (25%) and psychiatrists (19%). About 37% received mental health care from more than one type of provider.
“This reflects the important role primary care physicians play in the delivery of mental health care,” the researchers wrote, adding that it may also indicate difficulties accessing mental health specialists, “which needs exploring in future studies.”
The mean number of visits varied according to the type of mental health care provider, ranging from 2.1 for general practitioners to 4.6 for psychologists.
When the researchers compared patients who used mental health services with those who did not, they found that those who did were more likely to be separated, divorced, or widowed than married (22% vs. 17%), unemployed or on disability than employed (24% vs. 17%), and living in an urban setting than in suburban one (20% vs. 15%). They also had more years of education (15.4 vs. 14.8) and more were smokers (28% vs. 17%).
They experienced significantly worse symptoms of depression (9.1 vs. 5.8 points), anxiety (57.4 vs. 51.1 points), and fatigue (59.5 vs. 53.9 points). They also had lower self-efficacy for managing their disease (5.5 vs. 6.7 points), “which was previously shown to correlate with lower function and more emotional distress in SSc,” the researchers wrote.
Having higher education, higher anxiety symptom scores, limited SSc, smoking, and having lower self-efficacy were linked to more use of mental health services, an analysis showed. On the contrary, being retired was linked to less use of mental health services.
“Additional studies are needed to explore these factors,” the researchers concluded, adding that “the effects of these services in this unique patient population are also important to explore in future research.”
Among the study’s limitations, the team emphasized that SPIN participants may have higher access to specialized health care, including mental health care, than the general scleroderma population.