Case Report Reveals Divalproex Sodium Beneficial for Scleroderma Digital Ulcers
Written by |
 A case study of a patient with Scleroderma recently published in the journal JAAD Case Reports reports the clinical outcomes of treatment with HDAC (Histone deacetylase inhibition) with divalproex sodium.
A case study of a patient with Scleroderma recently published in the journal JAAD Case Reports reports the clinical outcomes of treatment with HDAC (Histone deacetylase inhibition) with divalproex sodium.
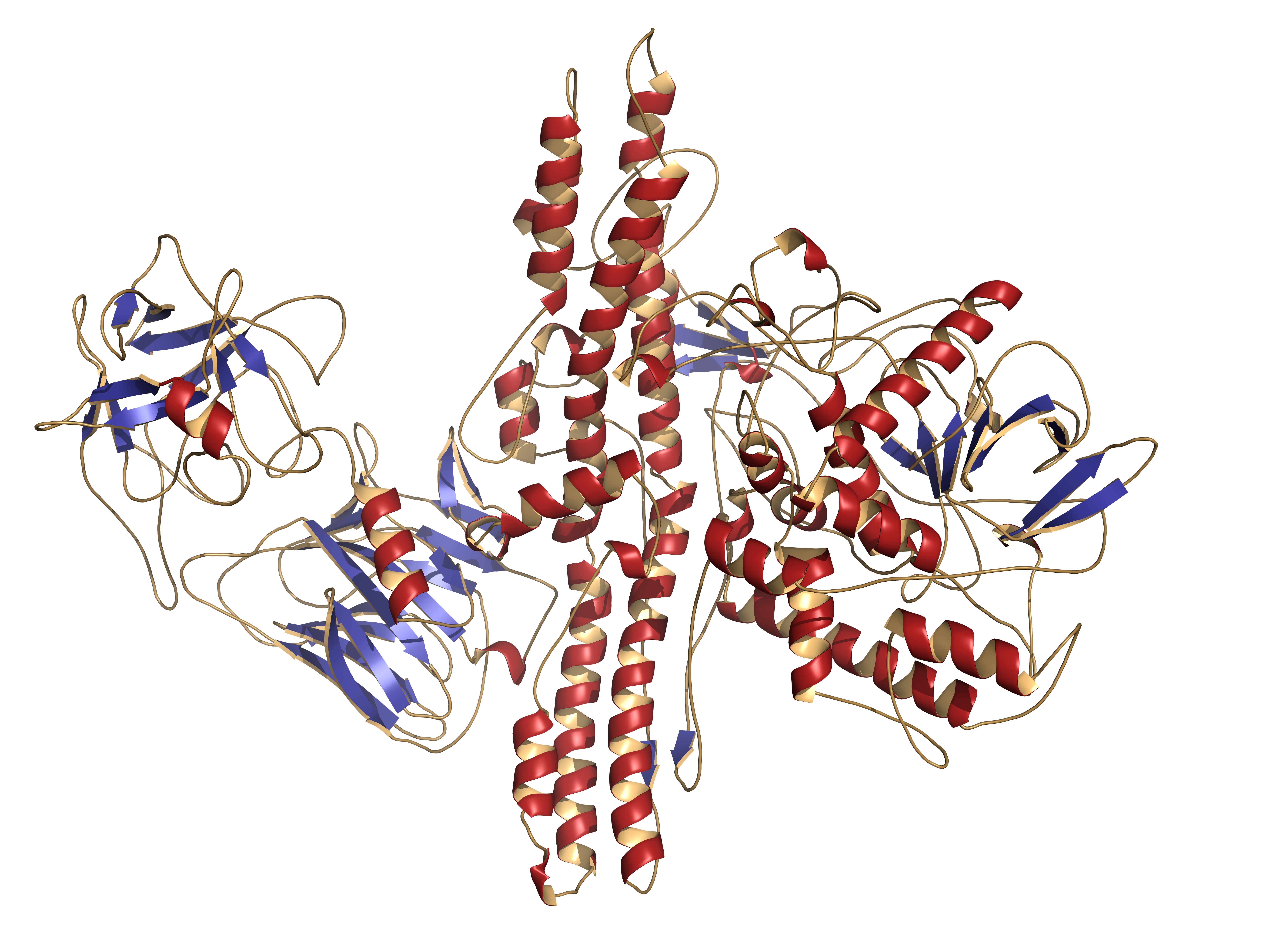
Scleroderma is a complex autoimmune connective tissue disease, and although the causes remain unclear, research suggests that transforming growth factor beta (TGF-β) is involved in the pathogenesis on the condition. Scleroderma involves the skin and internal organs, with manifestations usually including fibrosis and sclerodactyly, calcinosis cutis, digital ulcers, pigmentary changes, and telangiectasias. Recent evidence supports the notion that autoimmunity and inflammation, microvascular alteration, and fibrosis are the three pivotal pathways by which scleroderma occurs.
Immunosuppression and vasodilatory therapy are usually prescribed to patients to address the inflammatory and microvascular components of the disease.
In the study titled “Divalproex sodium: A potential therapy for scleroderma digital ulcers,” Jennifer R. Urban, BS from Stony Brook University School of Medicine in New York and Brett King, MD, PhD from the Department of Dermatology at Yale University School of Medicine in New Haven, Connecticut examined the efficacy of Histone deacetylase inhibitors (HDACi) on the antifibrogenic effects in the skin and other organs via mediation of transforming growth factor beta (TGF-β). In the report, they describe the case of a women aged 62 years with scleroderma. The patient presented with painful ulcers that involved the fingers. She had taken a regimen of rituximab, hydroxychloroquine, nifedipine, lisinopril, colchicine, aspirin, prednisone, and gabapentin for the symptoms’ recurrence, which happened every 2 to 4 months.
[adrotate group=”3″]
Upon clinical assessment, the clinicians observed the patient’s skin revealed pink-red erythema of the hands, peeling and fissuring of the palms and digits, and mild tapering of the distal fingers. They gave the patient divalproex sodium extended release 250 mg daily. After 4 months under the treatment, the patient did not experience digital ulcers and described reduced swelling of her fingers and also an improvement in her ability to grasp objects. Blood examinations did not reveal further problems. The clinicians questioned the potential benefit of divalproex sodium after the development of a digital pit, and because of this, the medication was discontinued after 6 months of treatment.
Within weeks of discontinuing divalproex sodium, the patient developed 4 painful digital ulcers. The clinicians decided to restart the treatment with Divalproex sodium ER 250 mg daily and they observed that the ulcers healed. After a follow-up of one and a half years, the patient is continuing to take divalproex sodium ER 250 mg daily and has had no recurrence of digital ulcers and presents a stable improvement in grasp function.
Based on these findings, the clinicians suggest that treatment with Divalproex sodium may be beneficial for the treatment of the digital ulcerations of scleroderma.





