Systemic Sclerosis Pathogenesis Appears Linked to Changes in Endothelial Cells, Researcher Tells SSc World Congress 2016
Scientists from the University of Florence, Italy, presented a study investigating the participation of the Endothelial-to-Mesenchymal transition (EndoMT) process in the pathogenesis of systemic sclerosis (SSc) at the 4th Systemic Sclerosis World Congress in Lisbon, Portugal, that concluded Feb. 20, 2016.
SSc is a chronic connective tissue disease characterized by the hardening and tightening of the skin. The proposed pathogenesis pathway involves the generation of myofibroblasts, whose dysregulated activity leads to excessive deposits of collagen and other proteins, and, consequently, fibrosis. Research indicates that these profibrotic myofibroblasts may arise from different sources, such as the expansion and activation of fibroblasts, the recruitment of circulating precursor cells, and the transition of epithelial cells into mesenchymal cells. It has also been suggested that endothelial cells (ECs) may transform into more myofibroblastic-like cells through a process called EndoMT.
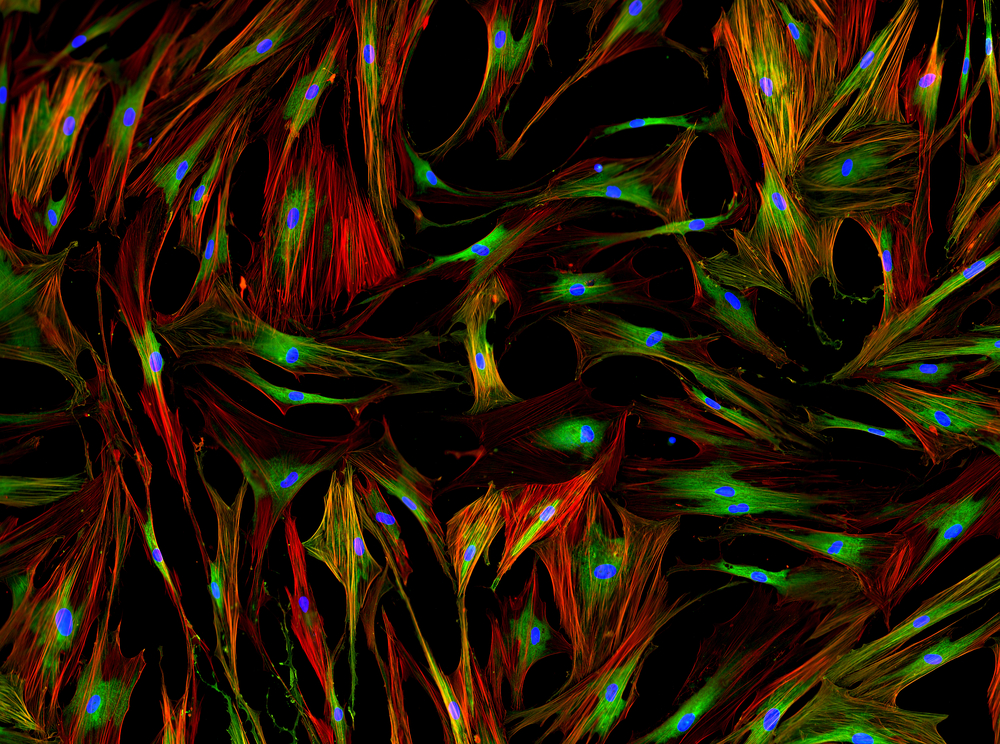
During EndoMT, ECs disaggregate, losing polarity and specific markers, and acquire myofibroblastic features. EndoMT can be induced in vitro by the transforming-growth factor (TGF)-β. As noted by Dr. Manetti in the presentation, “EndoMT has been implicated in the pathogenesis of SSc-associated pulmonary fibrosis and pulmonary arterial hypertension.”
Researchers investigated if EndoMT is an active participant in the pathogenesis of dermal fibrosis in SSc. The scientists collected skin samples from six patients with diffuse cutaneous SSc and six healthy subjects, and subsequently isolated dermal ECs. The expression of several markers characteristic of ECs or mesenchymal cells were evaluated. Skin sections of SSc patients and healthy subjects were also examined through immunostaining techniques.
According to the results presented at the congress, while dermal ECs from healthy controls exhibited expected and typical EC morphology, ECs derived from SSc patients had unusual elongated forms. While both cell samples had expression of EC biomarkers, the expression was significantly decreased in ECs derived from SSc patients. Moreover, the ECs from SSc patients expressed mesenchymal biomarkers, such as type I collagen, which were almost undetectable in ECs from the control group. The immunostaining assays and histological assessment of skin sections confirmed the presence of EC transformation only in SSc samples.
“Our findings provide the first direct evidence that EndoMT may contribute to the development of dermal fibrosis in SSc,” concluded Dr. Manetti on the presentation, suggesting that EndoMT might offer new potential therapeutic targets for SSc treatment.






