Protein, Netrin-1, Seen to Promote Lung Fibrosis in Early Scleroderma Study
In the lung’s extracellular matrix (ECM) — observed in both cultured cells from systemic sclerosis patients and a mouse model — the protein netrin-1 was seen to regulate the accumulation of collagen-producing fibrocytes and promote pulmonary fibrosis. The study, “Netrin-1 Regulates Fibrocyte Accumulation in the Decellularized Fibrotic Sclerodermatous Lung Microenvironment and in Bleomycin-Induced Pulmonary Fibrosis,” published in the Arthritis & Rheumatology journal, suggested netrin-1 as a potential new target for scleroderma-associated lung fibrosis.
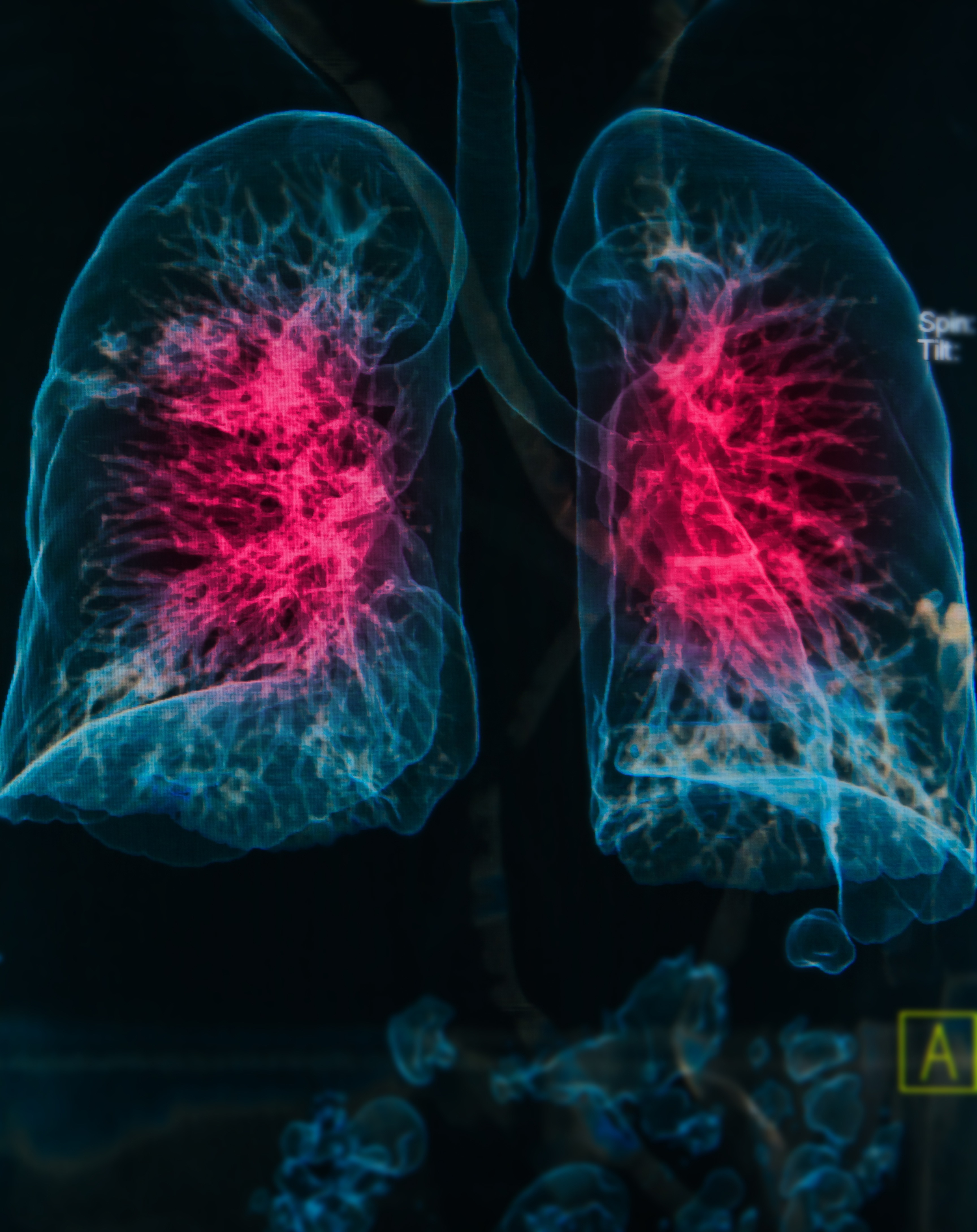
Systemic sclerosis, also known as scleroderma, is a chronic autoimmune disease characterized by excessive collagen deposits, leading to fibrosis in several internal organs. Fibrocytes are a particular type of cell circulating in the peripheral blood, which produce connective tissue proteins, such as collagen. These cells are known to accumulate in patients with systemic sclerosis affected by interstitial lung disease (ILD). However, how fibrocytes contribute to the disease and the factors regulating its appearance remain largely unknown.
A team of researchers investigated how ECM (a mesh of secreted proteins crucial in providing structural and biochemical support to cells within organs) in the lungs of scleroderma patients controls fibrocyte development. The team specifically investigated whether human lung ECM regulates collagen-producing fibrocyte-like cells in cultured human peripheral blood mononuclear cells (PBMCs).
To this end, researchers used a novel translational platform, a 3-dimensional model of the fibrotic lung microenvironment constructed from decellularized lung explants from control subjects and patients with systemic sclerosis-related ILD. Decellularization is a process to isolate the ECM of a tissue from its inhabiting cells, leaving an ECM scaffold.
The team found that both biochemical and mechanical parameters of the human lung ECM regulate the accumulation of collagen-producing fibrocytes. Moreover, researchers observed that PBMCs from patients with systemic sclerosis-related ILD showed increased responsiveness to components of decellularized fibrotic lungs. Focusing on a specific molecule, netrin-1, researchers found its expression to be increased in cells from patients with systemic sclerosis-related ILD. When using a mouse model of bleomycin-induced pulmonary fibrosis, the team observed that partial depletion of netrin-1 improved mice fibrosis.
Results suggested that factors in systemic sclerosis lung ECM regulate fibrocyte accumulation via a netrin-1-dependent pathway. Netrin-1, the researchers reported, is a possible therapeutic target for systemic sclerosis-related ILD.






