Autologous Hematopoietic Stem Cell Transplantation for Scleroderma Becomes Sought-After Treatment
Written by |
 Scleroderma patients from Canada are seeking access to an experimental U.S. stem cell therapy to help fight the disease. A study pioneered by Dr. Richard Burt at Northwestern Memorial Hospital in Chicago features injecting stem cells intravenously, in an approach called Autologous Hematopoietic Stem Cell Transplantation (HSCT).
Scleroderma patients from Canada are seeking access to an experimental U.S. stem cell therapy to help fight the disease. A study pioneered by Dr. Richard Burt at Northwestern Memorial Hospital in Chicago features injecting stem cells intravenously, in an approach called Autologous Hematopoietic Stem Cell Transplantation (HSCT).
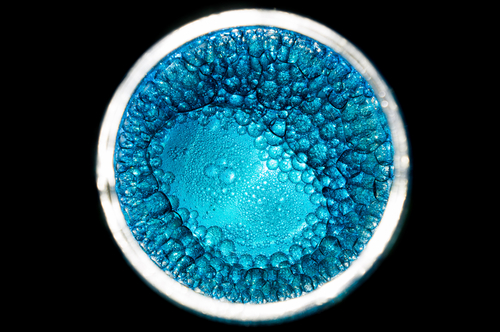
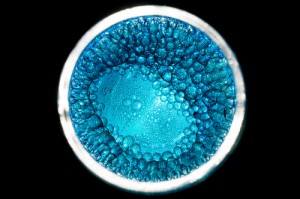
HSCT therapy begins by harvesting a patient’s own stem cells. Since Scleroderma, also known as systemic sclerosis, is a chronic systemic autoimmune disease (autoimmune diseases are characterized by a hyper-reactive response of the immune response against substances, and tissues normally present in the body), the second step of the therapy involves the use of chemotherapy to destroy the patient’s hyper-reactive immune system. Afterward, harvested stem cells are injected back into patients. The objective is to reset the patient’s immune system to normal standards and thus stop scleroderma. Although experimental, in a previous study published in the journal Lancet in 2011, researchers found that the therapy improved skin and pulmonary function in scleroderma patients for up to two years. In agreement, many patients reported that disease progression stopped after therapy.
The treatment, however, is considered experimental and is not available in Canada. Moreover, Ontario’s provincial health insurance does not cover those patients who would like to access to the therapy in the US.
As such, several Canadian patients have begin crowdfunding campaigns to pay for the treatment. The first scleroderma patient was Erin Zubick, who after none of the current treatments helped her in Canada, decided to get the stem cell therapy in the U.S with money fundraised in an online fundraising campaign.
Erin Zubick commented in a report for CTV News on the benefits of HSCT treatment: “Actually, when I was in the hospital even, my skin started to soften. I’m able to live a very normal life; I’m able to keep up with the kids. I’m able to go to school; and I’m off a lot of medications.” Now, a year later after treatment, Erin Zubick reported remarkable benefits of the therapy and she believes her disease is in remission.
A new Canadian patient, Mike Berry of Kingston, Ontario, also diagnosed with scleroderma, described to CTV News his daily life with scleroderma: “I’m unable to work any longer; it affects me and everything now. It’s hard to walk fast; I can’t walk and talk.” Now, Mike Berry is following Erin Zubick’s steps and started a fundraising campaign to get access to the HSCT therapy in the US.
In Canada, however, the medical community is still reluctant and notes that more research is required before HSCT can be introduced as a standard therapy. The treatment was associated with a higher death risk mortality in the first year after treatment, according to a European study. However, this risk declined within one year of treatment.
Dr. Janet Pope, chief of rheumatology at St. Joseph’s Health Care Centre in London, Ontario commented, “It is basically a dangerous procedure where 1 in 10 can die in the first year, and only very few people with scleroderma are eligible for the treatment. It’s something that’s really not appropriate at this point in time. I think we’ll know more over time, but it’s not ready for primetime for all of our patients in Canada. It’ll never be ready for primetime for most of our patients in Canada with scleroderma.”





