Systemic Sclerosis Patients at Threefold Risk for Venous Thromboembolism
Written by |
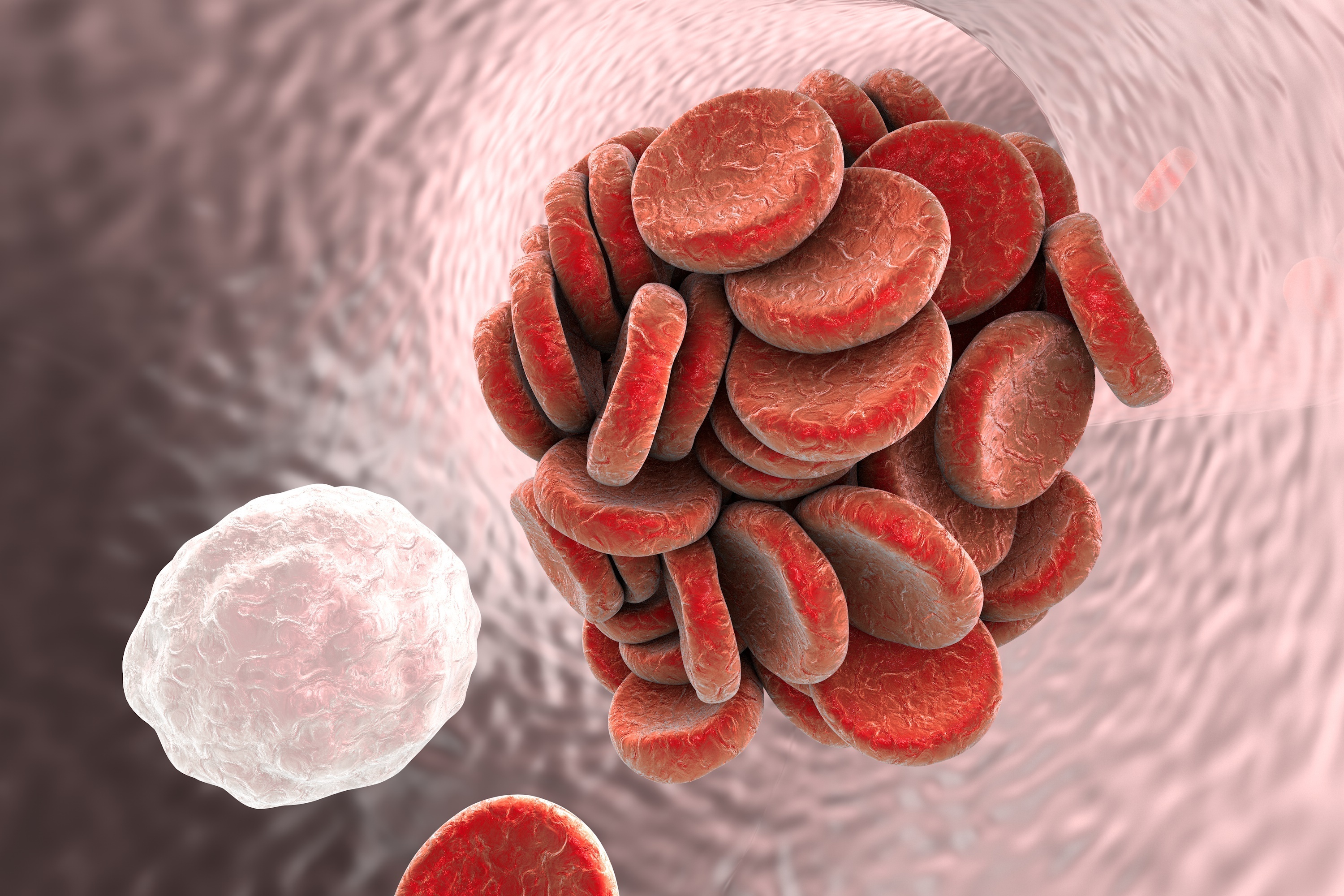
Systemic sclerosis (SSc) patients are at a substantially increased risk for the development of venous thromboembolism (VTE, obstructing blood clots), including pulmonary embolism (PE) and deep vein thrombosis (DVT), a study reported. The study, “Risk of Pulmonary Embolism and Deep Venous Thrombosis in Systemic Sclerosis: A General Population-Based Study,” was published in the journal Arthritis Care & Research.
VTE is known to occur more often among patients with inflammatory autoimmune diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and Behcet’s disease. Endothelial dysfunction can also contribute to the increased risk of VTE. SSc is an autoimmune disease without known etiology that manifests in several organs as vasculopathy and progressive fibrosis.
Vascular injury and endothelial dysfunction are important pathophysiologic features of SSc, as are pulmonary hypertension, renal crisis, and gastric antral vascular ectasia. Several studies on SSc hospital cases in Taiwan reported an increased risk of VTE, with one exception, where the risk of PE during the first year after admission for SSc increased but then declined. A better understanding of the possible increased VTE risk in this patient population is crucial to improving patients’ clinical outcomes.
Sara R. Schoenfeld and colleagues evaluated the risk of PE, DVT, and VTE according to SSc duration based on data from an unselected general population database that includes all residents of British Columbia, Canada. In total, 1,245 SSc patients (83 percent female, mean age of 56) were assessed.
Researchers found that SSc was associated with a threefold increased risk for PE, DVT, and VTE, particularly in the first year following SSc diagnosis. Interestingly, hospital-based studies do not seem to as strongly support the association of PE and VTE with SSc, probably due to biased patient selection and small population size.
Given the strengths and limitations of the study — a large population database capturing both primary care physician and specialist records, and both mild and severe cases of SSc — the results can be generalized. The potential limitations are inherent to all observational studies, like inaccurate diagnosis by using only International Coding Disease data.
Because this general study demonstrated that SSc is associated with a threefold increased risk of PE, DVT, and VTE, especially during the first year after SSc diagnosis, it indicates that increased monitoring for VTE risk factors among patients with SSc is required, regardless of recent hospitalization.
Patients with SSc experience high morbidity, and have an overall 10-year survival rate between 66 percent and 82 percent.





