Study Suggests Optimal Systolic Pulmonary Arterial Pressure May Increase Systemic Scleroderma Patients’ Survival Time
Written by |
 A multi-national team of researchers attempting to find precise clinical indicators that would increase post-diagnosis survival times among patients living with systemic scleroderma (SSc), have recently published a study with promising conclusions. The study consisted of patients previously diagnosed with SSc from the European League Against Rheumatism Scleroderma Trial and Research (EUSTAR) cohort. The aim of the study was to determine the predictive value of systolic pulmonary artery pressure (sPAP) using echocardiography. The study was published in the new issue of Rheumatology.
A multi-national team of researchers attempting to find precise clinical indicators that would increase post-diagnosis survival times among patients living with systemic scleroderma (SSc), have recently published a study with promising conclusions. The study consisted of patients previously diagnosed with SSc from the European League Against Rheumatism Scleroderma Trial and Research (EUSTAR) cohort. The aim of the study was to determine the predictive value of systolic pulmonary artery pressure (sPAP) using echocardiography. The study was published in the new issue of Rheumatology.
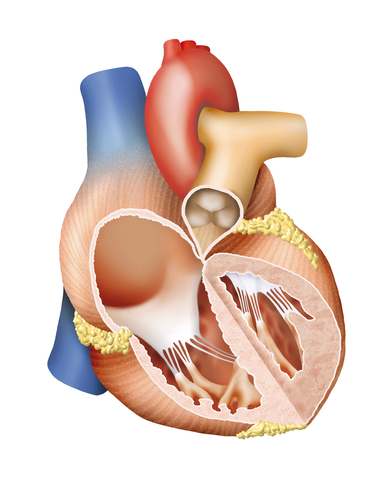
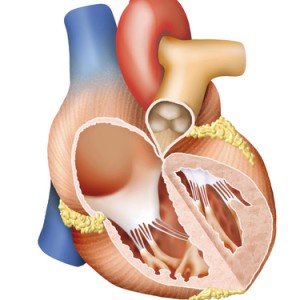
SSc is one of two types of conditions that make up the clinical diagnosis of scleroderma. SSc is a rare chronic disease that affects 75,000 to 100,000 people in the U.S. and is found at higher rates within populations of European ancestry. SSc causes a build-up of hardened scar tissues that result in damage to the body’s internal organs. Organ damage causes a myriad of problems for patients, ranging from kidney disease to life-threatening respiratory dysfunctions, such as interstitial lung disease. The cause of SSc is unknown, but researchers are confident that it is likely attributed to a genetic abnormality as opposed to an environmental cause. Presently there is no cure for SSc; however, there are drug treatments that help alleviate many symptoms associated with the disease.
The study’s authors chose to measure pulmonary arterial hypertension (PAH), commonly known as high blood pressure in the arteries of the lungs, for it contributes to a high percentage of disability and death in SSc patients. The three year survival rate among SSc patients with PAH who do not receive medical intervention is only 50-60%. PAH is often undiagnosed until patients are in the advanced stages of SSC which contributes to this high mortality rate.
[adrotate group=”3″]
The study analyzed data from 1476 SSc patients who had previously consented to be part of EUSTAR. Researchers chose to include a higher proportion of female patients (87%) in the study, in order to emulate the higher proportion of females that have been diagnosed with SSc, as compared to males. They looked at multiple clinical characteristics, including specific ranges of pulmonary arterial pressure, to determine which ranges could be highly successful in predicting reduced survival times for SSc patients. It was found that a sPAP greater than 36 millimmeters of mercury (mmHG) is highly indicative of lowered survival times in patients, regardless of whether they were previously diagnosed with PAH.
The results of this study will add to the growing body of knowledge that is assisting healthcare providers to accurately screen SSc patients for potential attributing risks that would significantly reduce their survival time.





