Sex differences confirmed in SSc, with 5 times higher risk for women
South Korean study ID subgroups, such as middle-aged women, most at risk
Written by |
Women have a nearly fivefold higher risk of developing systemic sclerosis (SSc), according to the findings of a nationwide study in South Korea that confirmed sex differences in the chronic autoimmune disease also known as scleroderma.
The higher risk of SSc for females versus males was more notable in several subgroups, specifically among middle-aged women and those who do not exercise regularly, the researchers noted. A greater risk also was seen for women without high blood pressure, known as hypertension, or any alteration of blood fat, or lipid, levels.
“These data are clinically meaningful as they provide comprehensive information that can lead to a better stratification of the risk of incident SSc in the perspective of sex,” the team wrote.
The researchers suggested that the increased risk “could be attributable to estrogen,” a hormone that plays a role in both the male and female reproductive systems but is found at much higher levels in women.
The study, “Sex differences in the risk of incident systemic sclerosis: a nationwide population-based study with subgroup analyses,” was published in the journal Scientific Reports.
Higher risk of SSc seen for women not exercising regularly
SSc is characterized by inflammation and fibrosis, or the accumulation of scar tissue, in the skin and internal organs, including the heart, lungs, and kidneys. Most commonly, the disease develops in people in their 30s and 40s, and in women.
However, according to the researchers, “although higher prevalence of SSc in women than in men is well-known, it is still unclear to what degree the risk of developing incident SSc is higher in women than in men.”
To address this knowledge gap, the team, from Seoul, analyzed a Korean nationwide database involving 9,894,996 individuals, followed between 2009 and 2019. A slight majority were men (54.6%).
The women were older than the men (48.8 vs. 46 years) and more commonly had low income (in the lower quartile; 19.8% vs. 11.9%). They also had lower body mass index, or BMI, a measure of body fat based on weight and height, and lower blood pressure. Females in the database also had a lower estimated glomerular filtration rate — a marker of kidney damage — and were less likely to have type 2 diabetes. Conversely, women more frequently had increased blood levels of cholesterol and triglycerides, a type of fat.
The researchers noted that the proportion of nonsmokers (94.7% vs. 30.4%) was higher among women, as was the proportion of participants who did not drink alcoholic beverages (74.9% vs. 32.5%), and those who performed regular exercise (15.6% vs. 19.9%).
During a mean follow-up of 9.2 years, 1,355 participants developed SSc, corresponding to a total incidence rate of 1.49 per 100,000 person-years. As a measure, person-years take into account both the number of people in a study and the total time each individual spends in the study.
The data showed the incidence of SSc was higher in women than in men (2.69 vs. 0.48 per 100,000 person-years).
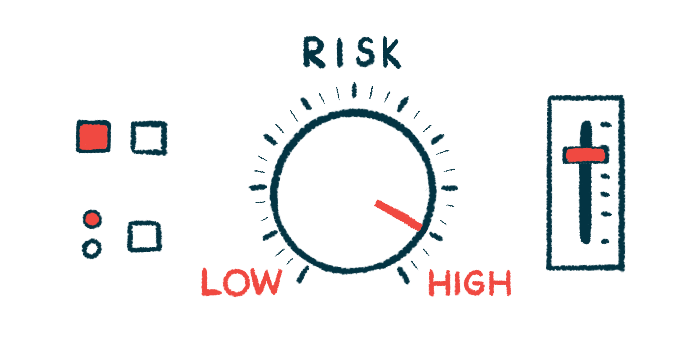
Considering that women have a higher risk of developing SSc, these subgroups of women should be stratified as having a very high risk of incident SSc.
Further analysis indicated that women had a nearly five times higher risk of developing SSc, which was consistent after adjusting for age, income, and a number of health parameters. Among them were smoking status, alcohol consumption, physical activity, and BMI. The analysis also took into account coexisting conditions such as type 2 diabetes, hypertension, altered blood fat levels, and chronic kidney disease.
“The higher risk of … SSc in women than in men was more prominent in several subgroups of individuals, including those aged 40-64 years, those without abdominal obesity, those who do not exercise regularly, [and] those without hypertension,” the researchers wrote.
A subgroup analysis found the higher incidence of SSc in women to be more pronounced in those in middle age compared with those younger than 40 and those 65 and older. A high risk was also seen for women not regularly exercising.
“Considering that women have a higher risk of developing SSc, these subgroups of women should be stratified as having a very high risk of incident SSc,” the researchers wrote.
The researchers suggested that estrogen may be linked to the likelihood of developing the condition, noting that “as women have higher levels of estrogen than men, this may have led to a higher risk of incident SSc.”