Restoring CCN3 Protein in Skin Could Improve Growth of Blood Vessels in Scleroderma, Study Suggests
Written by |
Restoring the levels of a protein known as CCN3 in the skin of people with scleroderma may improve the growth of new blood vessels and become a therapeutic target in this chronic disorder, a new study suggests.
The study, “Decreased CCN3 in Systemic Sclerosis endothelial cells contributes to impaired angiogenesis,” was published in the Journal of Investigative Dermatology.
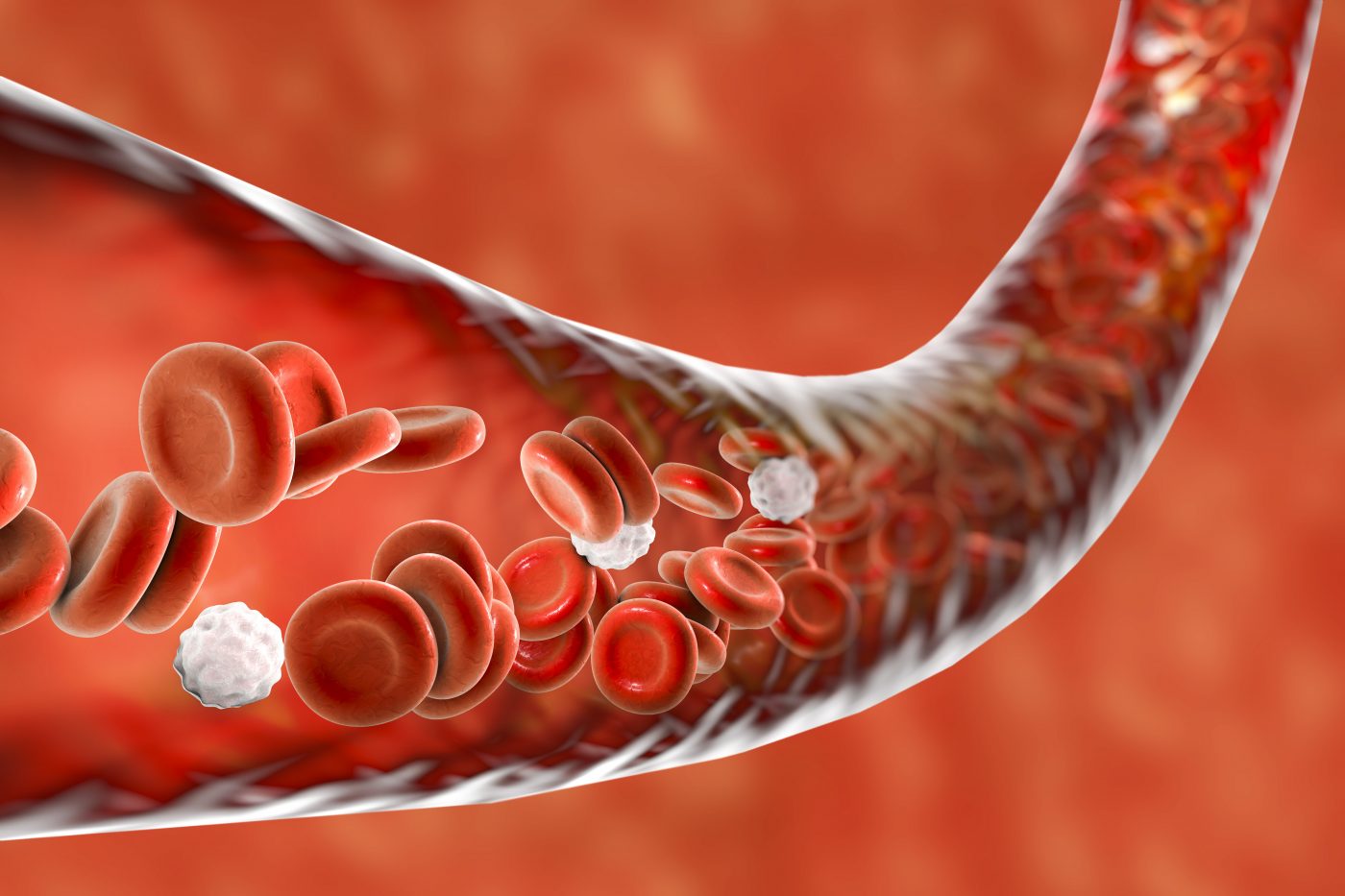
Raynaud’s phenomenon — a condition in which the fingers and toes feel numb, prickly, and frigid due to cold temperatures or stress — is usually the first manifestation of vasculopathy, or a disease affecting blood vessels, in people with scleroderma. Other manifestations affecting blood vessels, such as pulmonary hypertension, are silent at an early stage.
One of the major challenges of scleroderma-associated vasculopathy is to identify new therapeutic targets.
CCNs are a family of proteins involved in several cellular pathways associated with the development and progression of scleroderma. One member of this family is CCN2, a well-known promoter of fibrosis, or scarring in scleroderma. CCN3, which contributes to the formation of blood vessels, is regarded as a blocker of CCN2.
As such, a group of researchers from France sought to determine whether CCN3 is altered in the skin of people with scleroderma and if it could be a therapeutic target.
The team collected skin biopsies from 26 people with scleroderma, which included both fibrotic and non-fibrotic areas in 17 patients. They also collected samples from 18 healthy people (controls).
The results showed that the thickness of the superficial dermis — the skin layer underneath the top layer, called the epidermis — was significantly decreased in both fibrotic and non-fibrotic skin areas of people with scleroderma compared with healthy controls. This finding was observed even at early stages of the disease, meaning less than one year following diagnosis.
The number of blood vessels also was lower in both skin areas of the scleroderma patients than in controls.
In addition, scleroderma samples had lower CCN3 levels, and fewer cells containing CCN3 and CD34, the investigators found. CD34 is a protein marker of endothelial cells — those that line the interior of blood vessels — and cells surrounding dermal vessels.
Next, the researchers cultured — or grew in a lab — dermal endothelial cells from those with scleroderma and from the healthy controls.
Protein analysis revealed a significant decrease in cellular CCN3 levels in the scleroderma group. Still, administration of the pro-inflammatory molecule interleukin-1beta increased secretion of CCN3 in these cells. That suggests that the protein’s levels may be modulated, the researchers said.
The team also investigated the distribution of CCN3 within these cells. In the healthy controls, the protein was located both in the cytoplasm — the material inside cells, excluding the nucleus — and in the nucleus. In contrast, CCN3 was almost absent in the nucleus of cells from scleroderma patients. This suggests the protein is being retained in the cytoplasm, the team added.
Using an anti-CCN3 antibody to block this protein significantly impaired blood vessel formation, the scientists also found. Such use was associated with decreased cell migration, as assessed by the level of wound closure after eight hours.
In contrast, the use of engineered or recombinant CCN3 (rCCN3) improved angiogenesis — the growth of new blood vessels — in these cells, although it did not normalize wound closure.
“Altogether, these data show that rCCN3 partly restores the angiogenesis defect observed in [scleroderma cells],” the scientists said.
“CCN3 may represent a promising therapeutic target for SSc patients presenting with vascular involvement,” they concluded.





