Study links gut bacteria to severity of scleroderma-related ILD
Researchers enrolled 285 people with SSc to study gut bacteria, lung disease
Written by |
The presence and severity of interstitial lung disease in people with systemic sclerosis (SSc) are associated with a specific combination of bacteria in the gut, a study suggests.
“These species or their metabolic products may influence ILD [disease processes] and represent novel treatment targets,” the study’s researchers wrote. The study, “International Investigation of the Gut-Lung Axis in Systemic Sclerosis-Interstitial Lung Disease,” was published in Arthritis Care & Research.
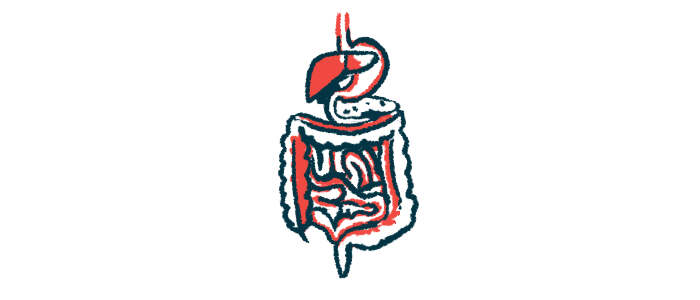
SSc, or scleroderma, is caused by an overactive immune system that leads to inflammation and the accumulation of scar tissue, or fibrosis, in the skin and internal organs. When fibrosis occurs in the lungs, it can lead to ILD, causing damage to the air sacs and making breathing difficult.
While people with SSc may have an imbalance in the gut microbial community, or intestinal dysbiosis, no studies have explored its relationship with SSc-ILD, leading researchers to study 285 scleroderma patients, who did or didn’t have ILD, from seven SSc centers on five continents. The participants had a mean age of 54.7 and a disease duration of 9.8 years. Most were women (83.5%) and 62.5% had ILD. Those with ILD were more likely to use proton-pump inhibitors (88% vs. 69%), which reduce stomach acid production, and immunomodulatory therapies (73% vs. 50%).
Exploring link between SSc-ILD, gut microbiome
The extent of ILD was determined through analyzing high-resolution CT chest scans and calculating a QILD score, where higher scores represent greater ILD extent. The researchers also analyzed the gut microbial composition by genetic sequencing of stool samples.
A total of 257 bacterial species were identified. After adjusting for current or prior treatments, body mass index (a measure of body fat that considers weight and height), and excessive growth of bacteria in the small intestine, 10 species were associated with ILD. Five were less abundant in SSc patients with ILD and the other five were more abundant.
This suggests “specific bacterial species and/or their metabolic products participate in ILD pathogenesis,” the researchers wrote.
The abundance of 18 bacterial species correlated with the participants’ QILD scores among 103 participants with SSc-ILD from two study sites.
Further analysis indicated the bacterial profile associated with ILD severity included 25 species. The species Dysosmobacter welbionis, GGB3005_SGB3996, and Anaeromassilibacillus sp An250 were associated with more severe ILD, but Anaerobutyricum hallii, Bifidobacterium adolescentis, and Streptococcus parasanguinis were associated with less severe ILD.
“A notable finding of this study is that SSc patients from geographically distinct areas of the world had a common repertoire of species that were specifically associated with ILD. The abundance of these species was increased across all patients with SSc-ILD, regardless of the study site,” the researchers wrote.
Fifteen biological pathways were associated with ILD severity, but not with the presence of ILD. These included glycogen degradation, a metabolic pathway by which the sugar molecule glycogen is broken down into glucose to provide energy to cells, and the urea cycle, a pathway in the liver that converts toxic ammonia into urea.
“Improving our understanding of the role of the [gastrointestinal (GI)] microbiome in ILD may reveal novel therapeutic strategies to modify the GI microbiome through diet, personalized pre- or pro-biotics, selective antibiotics, and/or specific bacterial transfers,” the researchers wrote.