Northwestern Researchers Find Immune Cells Link to Fibrosis, Reversing Previous Theories
Written by |
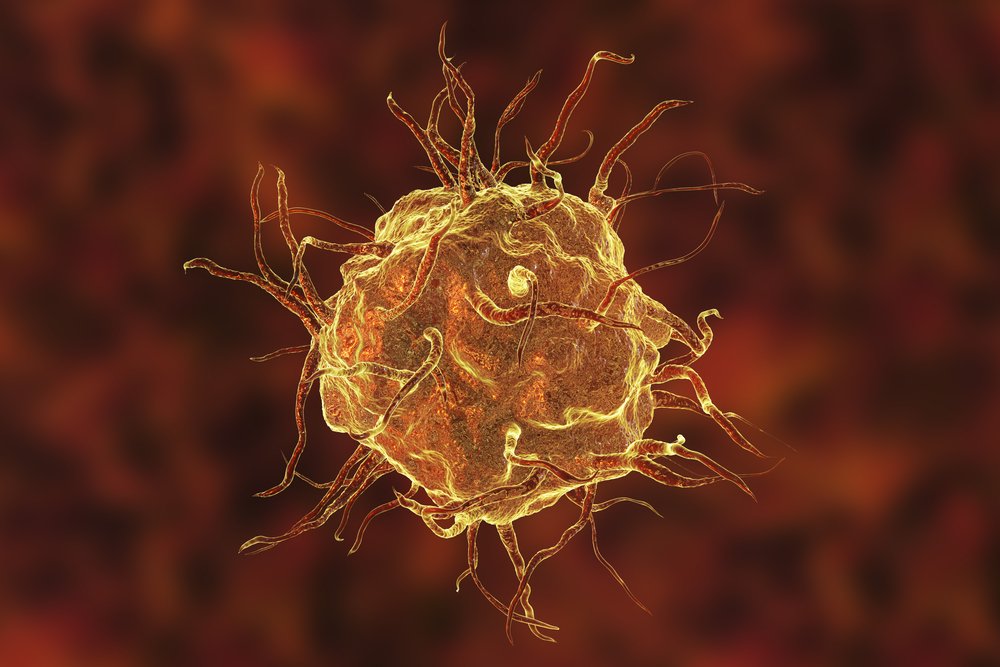
Certain immune cells contribute to the development of fibrosis, researchers at Chicago’s Northwestern Medicine discovered in a study that might overturn the view of lung fibrosis as a disease unaffected by immune processes.
The report titled, “Monocyte-derived alveolar macrophages drive lung fibrosis and persist in the lung over the life span,” suggests that by targeting these immune cells — called monocyte-derived alveolar macrophages — new fibrosis treatment options could be developed, including for idiopathic pulmonary fibrosis and scleroderma-associated pulmonary fibrosis.
The study was published in The Journal of Experimental Medicine.
Using both animal models of lung fibrosis and tissue from diseased and healthy lungs, the research team — led by Scott Budinger, MD, chief of pulmonary and critical care at Northwestern’s Department of Medicine, and Harris Perlman, PhD, chief of rheumatology at the department — traced immune cells through various disease stages.
They noted that so-called macrophages in the lung’s alveoli (air sacs) turned on a host of fibrotic genes in diseased tissue, but not in healthy tissue. Only macrophages derived from monocytes — a cell type that produces several immune cells — were involved. What researchers call tissue-resident macrophages — immune cells that stay in the tissue to govern normal processes — did not participate in the fibrotic processes.
The team validated their findings in both animal models and human tissue samples.
“One of the strengths of our study is that we go from bench to bedside,” Perlman said in a Northwestern news release written by Anna Williams.
The team also showed that the elimination of monocyte-derived macrophages prevented fibrosis development in mice.
“This will be transformative for the field,” said Alexander Misharin, MD, PhD, assistant professor of medicine at Northwestern Medicine’s Division of Pulmonary and Critical Care. “Pulmonary fibrosis is a complex disease — it’s not driven by a single gene or cell type — but this study now demonstrates that these immune cells play a key role. This will change the current paradigm.”
The research team used a method called next-generation sequencing to examine how different types of immune cells act as the disease progresses. The method can be used to study the transcriptome of a tissue or cell type. The transcriptome is the full set of mRNAs — intermediates between genes and proteins — produced in a cell, giving researchers a window into the full genetic activity of the cell.
“This is a novel application of genomic technologies to understanding pulmonary fibrosis,” Budinger said. “By showing that these technologies can be directly applied to patient samples, we offer the promise of incorporating them into personalized medicine approaches. It creates a resource for the research community to develop novel therapies.”
The researchers are now using the same approach to study lung tissue from patients with pulmonary fibrosis, fibrosis-affected skin from patients with scleroderma, and joint tissue from patients with rheumatoid arthritis to search for other immune mechanisms that drive fibrosis in these conditions.





