Exosome-based therapy eases skin scarring in scleroderma mice: Study
Findings could lead to new scleroderma treatment, researchers say
Written by |
Exosomes, tiny sacs containing biomolecules secreted from stem cells, thinned skin scarring in a mouse model of scleroderma, as well as skin samples from patients, a study reported.
These findings support “the use of exosomes as a clinical treatment for [scleroderma] skin fibrosis,” the researchers said in the study, “Exosomes carrying adipose mesenchymal stem cells function alleviate scleroderma skin fibrosis by inhibiting the TGF-β1/Smad3 axis,” which was published in Scientific Reports.
Scleroderma is an autoimmune disorder marked by the abnormal accumulation of collagen, the main protein component of scar tissue, in the skin and various organs. It’s called localized scleroderma when it affects just the skin and/or underlying muscle tissue, and systemic scleroderma when organs, including the heart, lungs, stomach, and kidneys, are also involved.
Nearly all scleroderma patients have skin involvement, and the severity of skin scarring, or fibrosis, is typically associated with damage to the vital organs and mortality.
Mesenchymal stem cells, or MSCs, are a type of stem cell found in various tissues, including the bone marrow, adipose (fat) tissue, and the umbilical cord. Due to their anti-fibrotic and anti-inflammatory properties, MSCs have been considered a promising treatment for scleroderma.
MSCs work by releasing signaling proteins and/or exosomes, tiny membrane-bound sacs that carry proteins and other molecules important for cellular communication. Because exosomes are cell-free, they may circumvent the adverse effects associated with MSC therapy, including immune rejection.
Study suggests AMSCs could hinder fibrosis
A research team at Fudan University in China tested whether exosomes derived from adipose tissue MSCs, or AMSCs, had the same effects on skin fibrosis as the parental AMSCs.
First, the team isolated fibroblasts, the connective tissue cells that produce collagen, from the forearm skin of five patients with diffuse scleroderma.
When AMSCs were cocultured with patient skin fibroblasts in direct contact for two days, several fibrosis markers, such as alpha-SMA, COL3A1, and TGF-beta1, were significantly reduced compared with fibroblasts alone. Even when a membrane separated cells to prevent direct contact, the markers were significantly reduced, suggesting AMSCs could inhibit fibrosis through secretions, the team noted.
Accordingly, exosomes derived from AMSCs also attenuated fibrosis in patient fibroblasts, significantly reducing all three profibrotic markers. Further experiments showed exosomes exerted their effects by suppressing the TGF-beta1/Smad3 pathway, a well-established pathway that promotes scar formation.
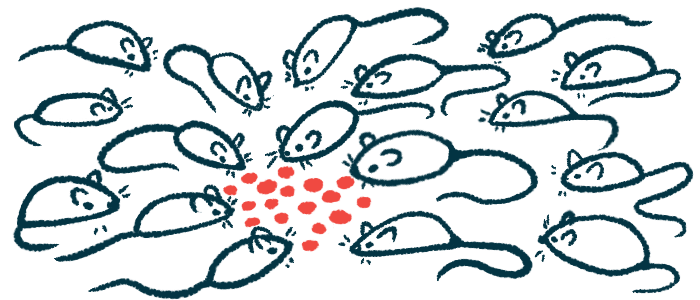
Next, the researchers injected AMSCs and derived exosomes under the skin of mice with chemically induced skin fibrosis, and tissues were examined one week later.
Skin staining showed the dermis, the inner layer of the skin, was significantly thinner, with fewer inflammatory cells and reduced collagen production in mice treated with AMSCs or exosomes compared with untreated mice. Direct measurements of the dermal layer thickness confirmed these findings.
In line with patient skin samples, elevated collagen production and profibrosis markers in mice with skin fibrosis were significantly attenuated after AMSC and exosome treatment. Either treatment also inhibited the TGF-beta1/Smad3 pathway in mice.
“Our study suggests that exosomes can act as a cell-free substance that can circumvent the adverse effects of AMSCs while delivering their biological functions to improve [scleroderma] skin fibrosis,” the team concluded.