PAH Medications, Tracleer and Opsumit, Seen to Block Fibrosis in Systemic Sclerosis in Early Study
Written by |
Two approved treatments for pulmonary arterial hypertension — Tracleer (bosentan) and Opsumit (macitentan) — can block a molecular pathway that promotes fibrosis in systemic sclerosis (SSc), and may be a potential therapy for these patients as well, according to an early study.
The study, “Bosentan And Macitentan Prevent The Endothelial-To-Mesenchymal Transition (Endomt) In Systemic Sclerosis: In Vitro Study,” was published in the journal Arthritis Research & Therapy.
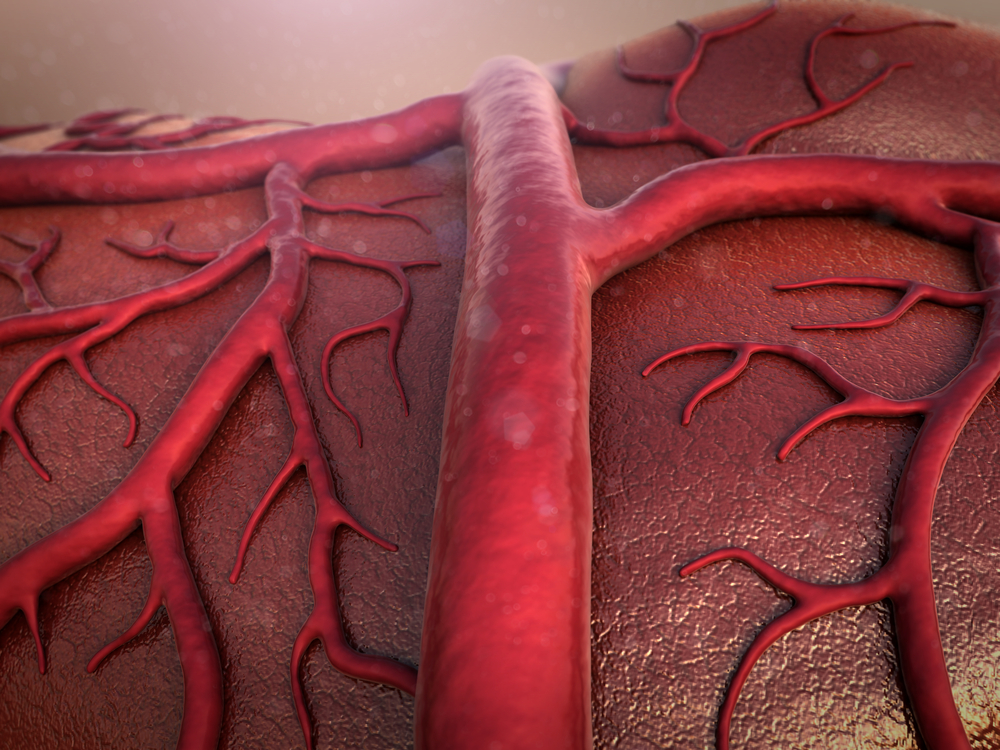
SSc is characterized by the development of fibrosis in the skin and other organs, and abnormal blood vessels. Although different molecules have been identified as key effectors of blood vessel rearrangement in SSc, such as ET-1 and TGF-β, the mechanisms underlying these abnormalities remain poorly understood.
Endothelial-to-mesenchymal transition, or EndoMT, is a complex biological process in which endothelial cells (cells that line blood vessels) lose their specific markers and acquire a fibrotic behavior. EndoMT can be induced by TGF-β, and this condition was recently associated with SSc development.
To understand the relationship between SSc and EndoMT, researchers took double skin samples (one from an affected area and another from a non-affected area) from 10 women with limited SSc. The team then prepared cultures of microvascular endothelial cells (MVECs) from the non-affected skin, together with fibroblasts from the affected skin. These fibroblasts were stimulated with two molecules that are considered to be mediators of fibrosis, ET-1 and TGF-β.
After two days in a culture, researchers analyzed the ability of MVECs to form tubes in the presence of SSc fibroblasts, as well as the expression levels of several molecules related to blood vessel formation (CD31, VEGF-A and VEGF-A165b) and pro-fibrotic activity (α-SMA, collagen type I, and TGF-β).
Results showed that, after 48 hours, MVECs showed a lesser tube formation ability in culture with SSc fibroblasts. Levels of factors that promote tube formation (CD31 and VEGF-A) were also lower, whereas VEGF-A165b, a protein that blocks the formation of blood vessels, was higher. Also, fibrotic markers such as α-SMA, collagen type I, and TGF-β were present in higher quantities.
Interestingly, cultures treated with the ET-1 receptor antagonists — Tracleer and Opsumit, which were approved by the FDA in 2001 and 2013, respectively — restored the tube formation ability of MVECs, and the balance in the expression of markers. This indicated that the TGF-β-induced release of ET-1 was behind the fibrotic response in MVECs, simulating EndoMT and contributing to the development of SSc, which was blocked by the drugs.
“The present study provides further in vitro evidence of the use of [bosentan and macitentan] in inhibiting the EndoMT process, supporting the clinical efficacy of these drugs in SSc therapy and their usefulness for interfering with progressive fibrosis,” the authors concluded.





