Autoantibody Profile in SSc Patients Can Help Predict Disease Outcome, Greek Study Finds
The prevalence of autoantibodies, particularly Anti-Topo I, anti-CENP, and anti-RNA pol III, in patients with systemic sclerosis (SSc) can aid in predicting disease outcome, Greek researchers have found.
Their study, “Disease-related autoantibody profile in patients with systemic sclerosis,” appeared in the journal Autoimmunity.
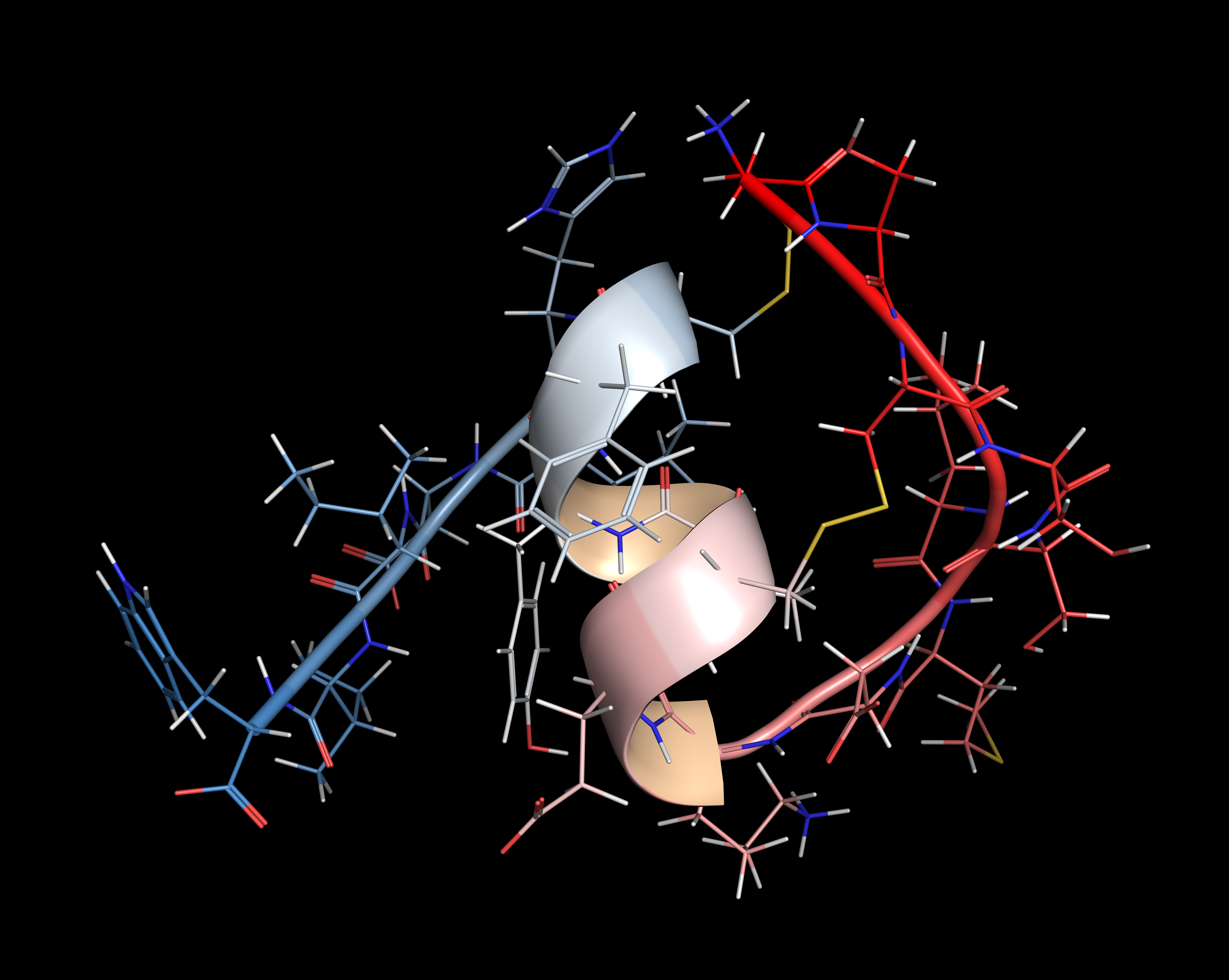
SSc is characterized by the presence of autoantibodies, which attack a patient’s own cells and tissues, contributing to the development of multiple autoimmune diseases.
Autoantibodies have been shown to play a role in SSc. The most common are anti-Topoisomerase I (anti-Topo I), which is associated with diffuse cutaneous SSc, and anti-centromere protein (anti-CENP), which is linked to limited cutaneous SSc.
Immunoassays, which can detect antibodies, have been useful in testing for the presence of several SSc-associated autoantibodies that can predict organ involvement and disease outcome.
Researchers at University General Hospital of Larissa, in the central Greek region of Thessaly, set out to determine the autoantibody profile of 13 SSc-specific autoantibodies in 131 Greek patients with SSc. Of the total, 49 had diffused cutaneous SSc and 82 had limited cutaneous SSc. Scientists used an immunoassay to detect autoantibodies.
Results showed that 89.3 percent of SSc patients were positive for at least one autoantibody. This included anti-Topo I (41.2% of patients); anti-CENP (28.2%); anti-RNA polymerase III, or RP11 (14.5%); anti-RNA polymerase IiI, or RP155 (9.9%); anti-fibrillarin (3.1%); anti-Ku (4.6%), anti-nucleolus-organiation region, or anti-NOR90 (6.1%); -anti-=pm-scl100 (1.5%) and anti-pM-Scl75 (3.1%).
In total, 77.9 percent of patients with SSc had autoantibodies against either Topo I, CENP, RP11 or RP155.
Upon further analysis, researchers found that the presence of anti-Topo I antibodies were significantly correlated to diffuse cutaneous SSc, interstitial lung disease (ILD), pulmonary hypertension (PH) and ILD-PH. Furthermore, anti-CENP antibodies were positively associated with limited cutaneous SSc, but negatively associated with ILD. Finally, the presence of the anti-NOR90 antibody was associated with ILD.
Researchers said conducting a profile of SSc-related autoantibodies may help evaluate and diagnose patients who have or may possibly have SSc, and that such a profile can allow physicians to predict the outcomes or potential comorbidities of ILD and PH in SSc patients.






