Raynaud’s Symptoms in SSc Seen to Ease with Iloprost and Bosentan Treatment
Written by |
Iloprost (brand name, Ventavis) in combination with bosentan (Tracleer) can improve blood flow in microscopic vessels called capillaries in the hands and feet of patients with systemic sclerosis, where poor capillary function often gives rise to Raynaud’s phenomenon.
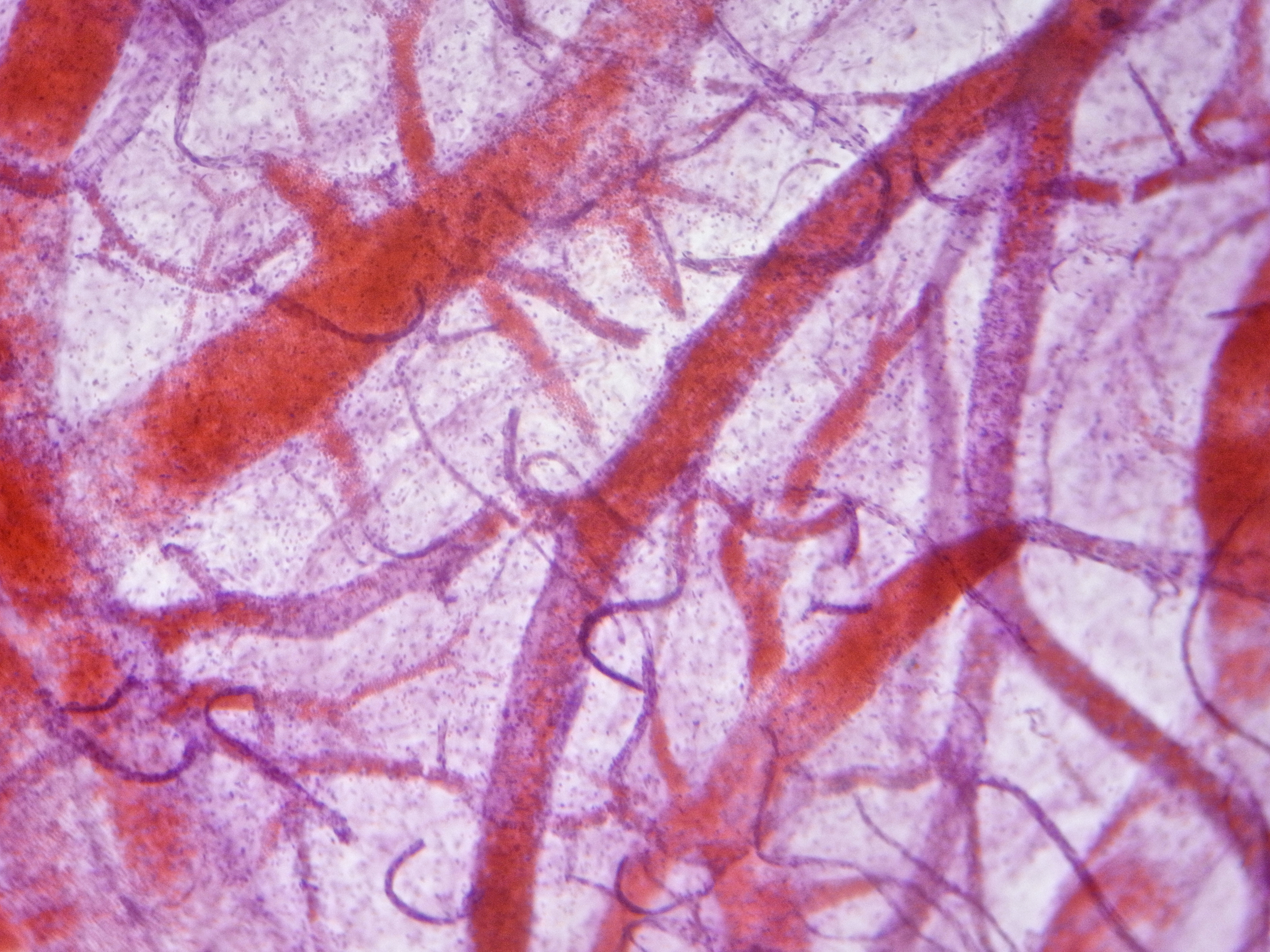
The study, “Effect of treatment with iloprost with or without bosentan on nailfold videocapillaroscopic alterations in patients with systemic sclerosis,“ recently published in the journal Modern Rheumatology, inspected capillaries at the nail fold of the finger using video microscopy to evaluate if the two drugs improve the workings of these blood vessels, potentially easing Raynaud’s symptoms.
Although a major focus in systemic sclerosis is the prevention of tissue fibrosis, poor blood flow in capillaries can lead to several complications, including Raynaud’s phenomenon, digital ulcers, scleroderma renal crisis, and pulmonary arterial hypertension. Raynaud’s is characterized by a feeling of numbness and cold, in response to low temperatures or stress, in such areas as the fingers and toes; it occurs because small arteries narrow, restricting blood circulation.
An earlier, large analysis of previously published studies showed that the drug iloprost, which dilates blood vessels and prevents blood platelets from aggregating, can reduce the severity of Raynaud’s. Bosentan, which is often used in combination with iloprost, has also shown beneficial effects on capillary function.
Researchers at the University of Modena and Reggio Emilia, in Italy, explored if potential changes in microscopic blood vessels in the hands and feet might be tracked with video microscopy of the nail folds, along with a system for scoring the architecture of blood vessels to assess risk for skin ulcers.
The study included 62 patients treated with iloprost alone, and 33 with iloprost and bosentan in combination.
After 12 months of treatment, researchers found that patients in the combination group had a statistically significant increase in ramified capillaries — blood vessels with extensive branching. Both groups also had fewer microbleeds and fewer numbers of giant capillaries, which are severely dilated vessels.
“Our study confirms the effectiveness of bosentan, in combination with iloprost, in SSc [systemic sclerosis] microangiopathy observed to NVC [nailfold videocapillaroscopy],” the authors concluded.
Although researchers noted some positive changes in the capillaries in both groups, they were not enough to significantly change the skin ulcer risk score. The score improved below the level of low risk in 9 percent of patients on combination treatment, while scores generally worsened in the group treated only with iloprost. Patients treated only with iloprost also had more digital ulcers at the end of the study.
The team believes that long-term studies should be conducted to determine the real-life, clinical effect of this therapeutic combination. “Given the short follow-up of 12 months, it is possible that the observed NVC changes might be better evaluated by long-term studies able to fully clarify the complex pathophysiological variations accompanying the clinical effects of combined bosentan and iloprost treatment,” the research team wrote.





