SSc Autoantibodies Associated with Malignancies
 Certain patients with systemic sclerosis (SSc) may be at a higher risk for malignancies based on autoantibodies present in their blood. Specifically, work presented by Dr. Cosimo Bruni at the 2014 American College of Rheumatology Annual Meeting, “An Association of Anti-PM/Scl Antibody Reactivity with Risk of Malignancy in Scleroderma,” described how these antibodies are associated with overlapping syndromes, including malignancy.
Certain patients with systemic sclerosis (SSc) may be at a higher risk for malignancies based on autoantibodies present in their blood. Specifically, work presented by Dr. Cosimo Bruni at the 2014 American College of Rheumatology Annual Meeting, “An Association of Anti-PM/Scl Antibody Reactivity with Risk of Malignancy in Scleroderma,” described how these antibodies are associated with overlapping syndromes, including malignancy.
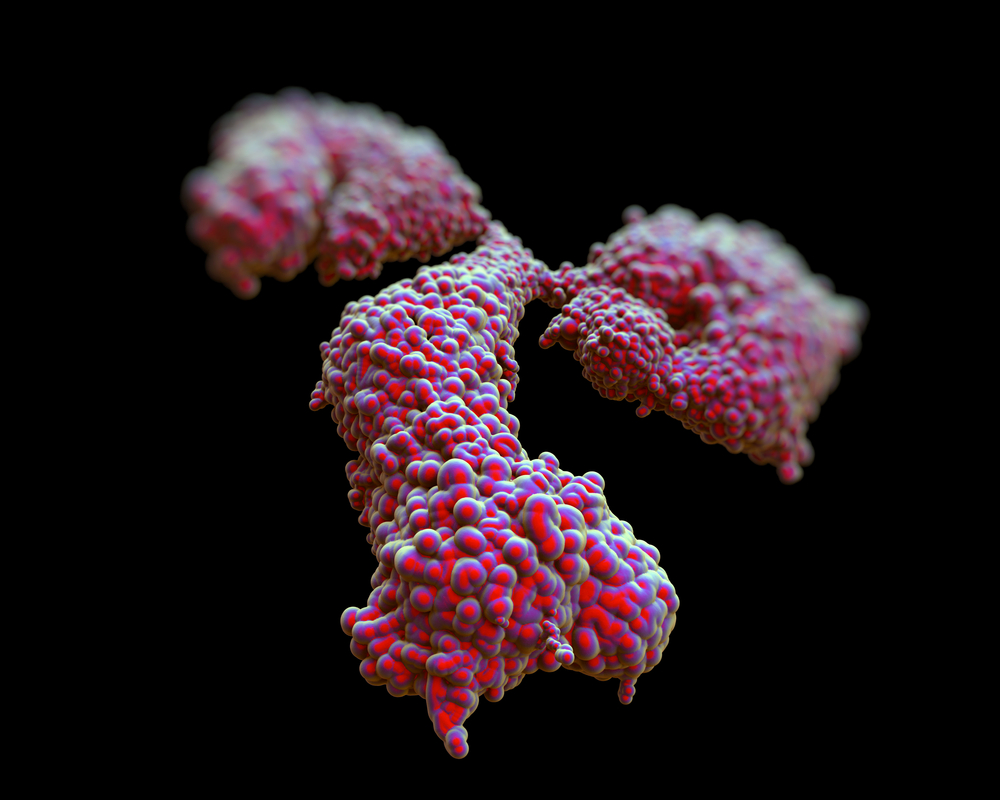
Anti-PM/Scl autoantibodies, which are specific for 75 kDa and 100 kDa human exosome components, are heterogeneous and common in patients with SSc. Up to 12.5% of patients with these autoantibodies also have myositis, mild skin involvement, pulmonary fibrosis, articular involvement, and calcinosis. Unlike some SSc patients, this cohort tends to have a lower prevalence of pulmonary arterial hypertension and gastrointestinal involvement.
Based on this range of clinical features, the authors of the study sought to describe the risk of malignancy in 2,200 patients from a single center cohort. The team identified anti-PM/Scl positive SSc patients through indirect immunofluorescence patterns and recorded clinical data concerning skin, internal organ involvement, and history of malignancy.
[adrotate group=”3″]
Overall, 70 anti-PM/Scl (3.1%) patients were in the cohort, and 48 patients had both PM/Scl 75 and 100 autoantibodies. This segment of the population frequently showed lung, gastrointestinal, and muscle involvement. Of greatest interest, there was a positive association between anti-PM/Scl 100 and malignancy, as opposed to both 75 and 100, or 75 alone. The population’s standardized incidence ratio for cancer was 2.14.
The most common malignancies identified in the group were breast and squamous cell adenocarcinomas, and the rest were haematological malignancies. According to the authors, “This cohort is otherwise representative of others in terms of demographics and clinical characteristics and underlines the importance of close surveillance for concurrent malignancy in all SSc disease subphenotypes.”






