Blood Test May Help Identify Systemic Sclerosis Patients at Risk of Poor Outcomes, Study Suggests
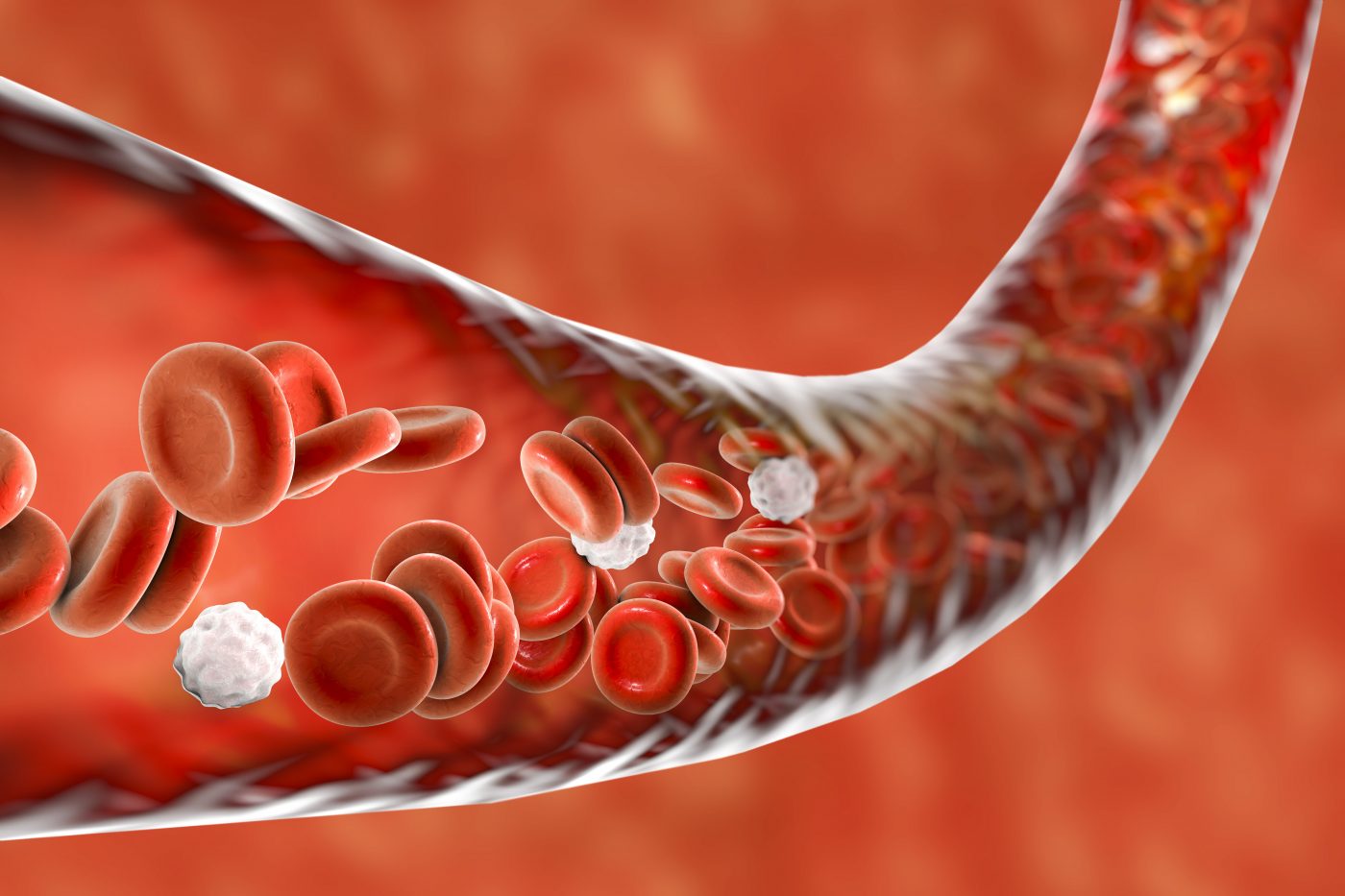
A simple routine blood test that measures the levels of immune cells called monocytes may help identify patients with fibrotic diseases, including systemic sclerosis, who are at risk for poorer outcomes, according to a study.
The study, “Increased monocyte count as a cellular biomarker for poor outcomes in fibrotic diseases: a retrospective, multicentre cohort study,” was published in the journal The Lancet Respiratory Medicine.
There is an urgent need for biomarkers that can help diagnose and predict the outcome of life-threatening fibrotic diseases, such as idiopathic pulmonary fibrosis (IPF) and systemic sclerosis.
A previous study had shown that an analysis of a panel of 52 genes in blood samples could successfully predict the outcome of patients with IPF. However, making this approach available for clinical practice would require “a substantial amount of work,” according to the researchers in the current study.
Several immune cell types, including monocytes, have been implicated in the development of systemic sclerosis and IPF, along with other fibrotic diseases. Nonetheless, immunosuppressive therapies tested in IPF clinical trials have failed to slow disease progression. In fact, clinical data suggested that inhibition of immune cells might even lead to shorter survival.
In this study, a team of researchers aimed to evaluate whether monocytes could help predict IPF patients at risk.
To test their hypothesis, they used patients’ blood samples and analyzed their monocyte content. They validated their results using electronic health records from additional groups of patients.
They started by looking at previously published genetic data to estimate the percentages of 13 types of immune cells, including monocytes, in 120 patients with IPF. They found that those patients who had a higher (above the mean) percentage of monocytes had a shorter lung transplant-free survival time.
Next, they analyzed the absolute count of monocytes by detecting the CD14 marker (which is specific for monocytes) in blood cells of 45 IPF patients from the COMET trial (NCT01071707). They saw that higher counts of CD14-positive monocytes corresponded to patients with progressive disease. Similarly, patients with IPF from another group had higher proportions of CD14-positive cells than healthy controls.
In this population, the team found that monocyte percentages were correlated with mortality risk. The six high-risk IPF patients were found to have more monocytes than the nine low-risk patients.
“We identified classical monocytes as a prognostic marker in patients with idiopathic pulmonary fibrosis,” the researchers wrote.
Next, the team analyzed the clinical records of 7,459 patients with fibrotic diseases stored at three publicly available databases — the Stanford Translational Research Integrated Database Environment, the Vanderbilt University Medical Center Database, and the Optum Clinformatics DataMart. With this information, they wanted to evaluate whether high monocyte counts were a prognostic marker of poor outcomes. An additional fourth database, Northwestern SSc ILD cohort, included data from 365 patients with systemic sclerosis.
Analysis further showed that, after adjusting for age and sex, IPF patients with monocyte counts of 950 cells per microliter of blood or higher were at an increased risk of all-cause mortality. Likewise, a higher absolute monocyte count was associated with shortened survival in patients with systemic sclerosis and other fibrotic diseases, including hypertrophic cardiomyopathy and myelofibrosis.
In control patients without IPF, monocyte counts had no predictive power for mortality. In addition, monocyte counts for individual IPF patients remained stable over time, indicating that their monocyte-derived risk profile was the same throughout time.
“Absolute monocyte count is a component of a complete blood count, a widespread and globally available routine clinical test, making this biomarker inexpensive and easy to implement,” the researchers wrote. Based on these findings, they believe that “absolute monocyte count at the time of diagnosis is a reproducible prognostic marker of poor outcomes in IPF and other fibrotic diseases.”
“Monocyte count should be incorporated into the clinical assessment of patients with IPF and other fibrotic diseases,” they suggested.






