Systemic Sclerosis May Be Linked to Changes in Gut Bacteria, U.S.-Norwegian Study Finds
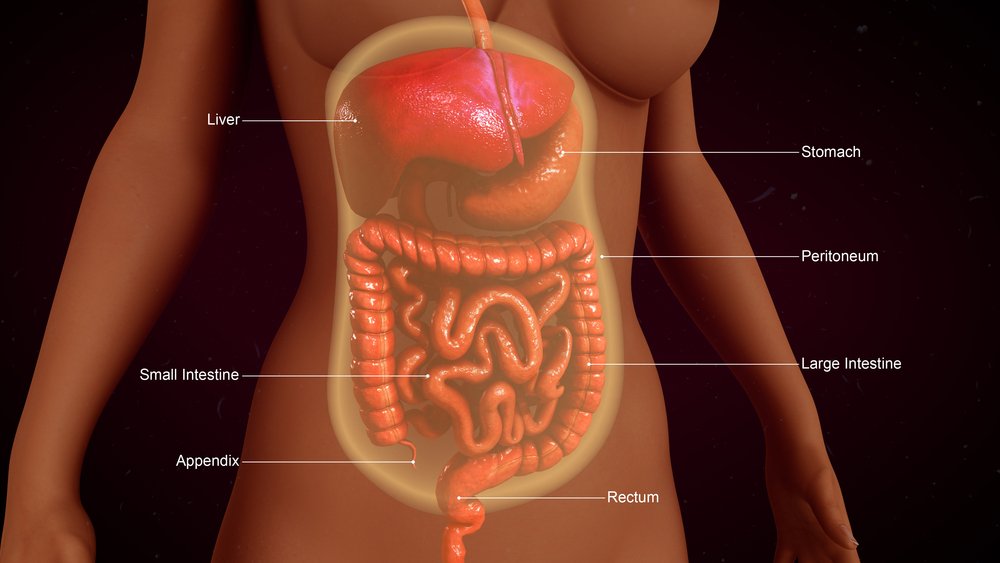
Systemic sclerosis (SSc) may be associated with changes in gut bacteria, according to a U.S.-Norwegian study which found that SSc patients are more prone to severe gastrointestinal tract (GIT) changes and symptoms.
The study, “Systemic sclerosis is associated with specific alterations in gastrointestinal microbiota in two independent cohorts,” appeared in the journal BMJ Open Gastroenterology.
GIT impairment affects more than 90 percent of SSc patients. However, the mechanisms underlying this condition are still largely unknown. The study aimed to find out whether GIT symptoms and SSc are caused by changes in bacterial populations present in the gut.
“Currently, few effective treatment options exist for managing lower gastrointestinal tract symptoms in patients with systemic sclerosis,” wrote the researchers. “If specific genera are found to contribute [to] the gastrointestinal tract phenotype in systemic sclerosis, such genera could provide specific targets for intervention to avert or treat this important clinical dimension of systemic sclerosis.”
The study included 17 adult SSc patients from the University of California Los Angeles (UCLA) and 17 from Norway’s Oslo University Hospital (OUH),as well as 17 healthy controls. Participants provided fecal samples, which researchers used to isolate and identify the bacteria species present. Results revealed that SSc patients had significantly lower levels of commensal bacteria such as Bacteroides (UCLA and OUH patients), Faecalibacterium (UCLA patients) and Clostridium (OUH patients). All are believed to protect against inflammation in the human body.
Interestingly, American patients had greater changes in gut bacteria than did the Norwegians. Patients also presented significantly higher levels of pathogenic bacteria such as Fusobacterium than did healthy individuals.
The analysis also revealed that higher levels of Clostridium were linked with less severe GIT symptoms in both groups of patients, meaning that specific bacteria species are associated with severe symptoms.
“Using two independent SSc cohorts, this study also uncovered relationships between specific [bacteria types] and severity of SSc-GIT symptoms, which merit further investigation,” researchers wrote. “While larger studies are needed to validate and expand on these findings, the present study is the first to characterize the lower GIT microbiota in two geographically and ethnically distinct SSc cohorts.”






