Stanford University Researchers Find Skin Cell Type Associated to Scarring
A new study recently published in the journal Science revealed that a specific skin cell type is associated to wound healing and scarring in mice. The study is entitled “Identification and isolation of a dermal lineage with intrinsic fibrogenic potential” and was conducted by researchers at Stanford University School of Medicine.
Fibroblasts are the main cell type responsible for collagen synthesis and the extracellular matrix of organs. Fibroblasts also have a critical role in wound healing as scars are mainly composed of collagen.
“We are the only species that heal with a pathological scar, called a keloid, which can overgrow the site of the original wound,” said the study’s co-senior author Dr. Michael Longaker in a news release.
Scars, either internal or external, can cause a serious burden, being linked to several medical conditions due to excess fibrous connective tissue (fibrosis). “The biomedical burden of scarring is enormous,” noted Dr. Longaker. “About 80 million incisions a year in this country heal with a scar, and that’s just on the skin alone. Internal scarring is responsible for many medical conditions, including liver cirrhosis, pulmonary fibrosis, intestinal adhesions and even the damage left behind after a heart attack.” Another serious scarring-related condition is scleroderma, a rare chronic autoimmune disorder where the body’s own immune system attacks healthy tissue resulting in a hardening and tightening of the skin and connective tissue (scarring).
In order to develop therapies for conditions related to fibrosis and scarring, it is necessary to better understand the pathogenesis and mechanisms associated to these processes. A previous study has reported two distinct lineages of fibroblasts in mice’s skin, where the one in the lower skin layer (characterized by the expression of a protein named engrailed) was found to regulate the initial repair steps in response to a wound.
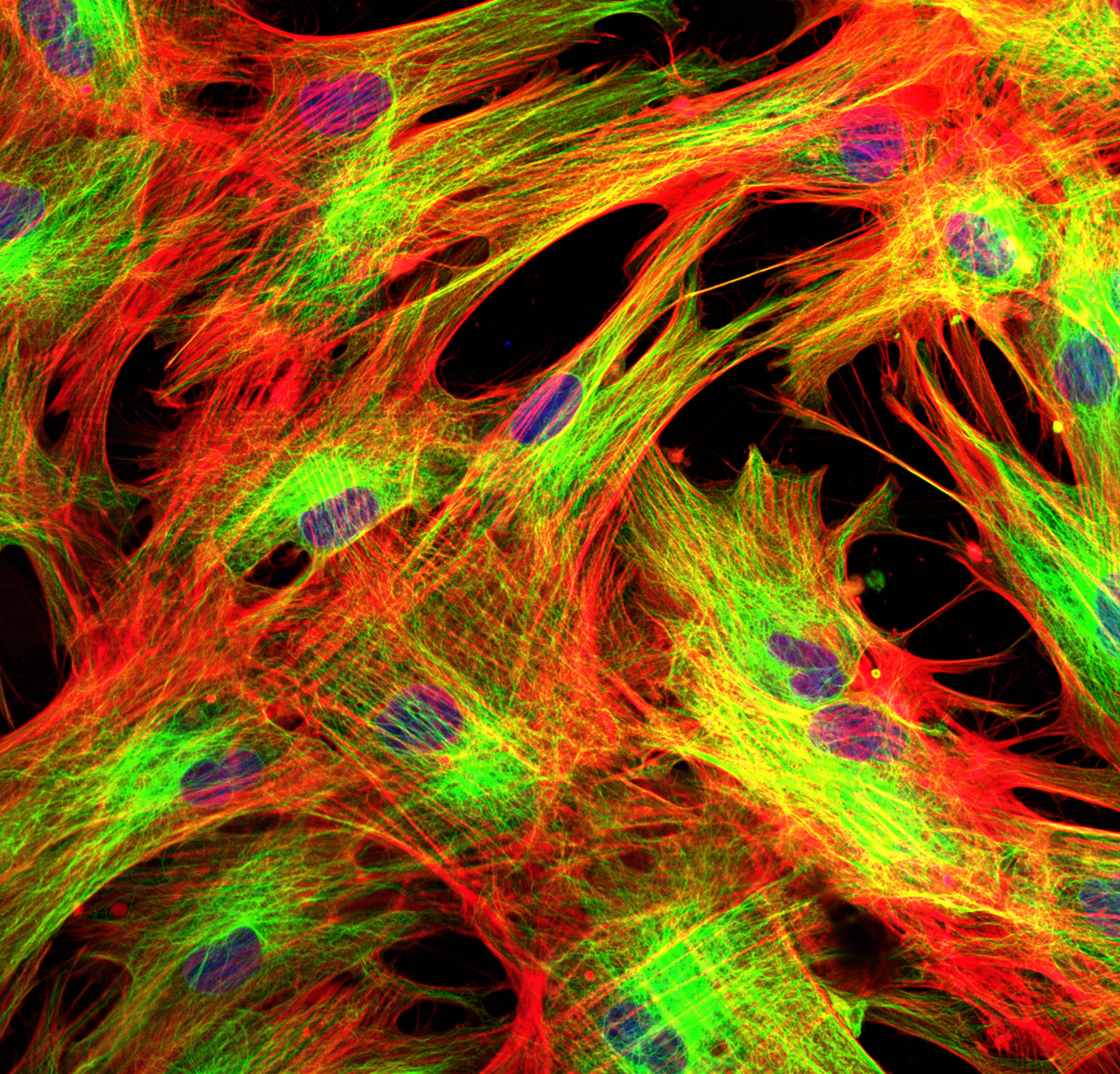
In this study, the research team hypothesized that this type of fibroblast, called “engrailed-positive fibroblasts” (EPF), could be responsible for collagen accumulation in the wound healing process and scar formation. Researchers genetically engineered mice in which EPF cells were tagged with a green fluorescent protein to allow their monitoring throughout mice development.
Researchers found that EPF cells in mice have a dramatic increase from less than 1% in embryos 10 days old to approximately 75% in animals 1 month old, in comparison to the overall number of skin fibroblasts. The team also found evidence that EPF cells play a crucial role in the scarring process, as in their absence, the wounds took an extra six days to heal completely but exhibited less scarring and a functional repaired skin.
The research team found that EPF cells express on their surface a protein called CD26, which has been linked to the metabolism of several hormones such as insulin, being used as a target in humans for type-2 diabetes. Blocking CD26 activity resulted in a slower wound healing in mice and a lessened scarring, similar to what is observed in the absence of EPF cells.
[adrotate group=”3″]
Researchers also found that these EPF cells are linked to radiation-induced skin damage (fibrosis) and melanoma growth (skin cancer), as in mice lacking EPF cells, fibrosis was considerably reduced after exposure to radiation and transplanted melanoma cells grew more slowly than in mice with normal EPF expression.
The research team concluded that skin EPF cells are responsible for scarring and possibly involved in radiation-induced skin damage and melanoma growth. The team suggests that targeted inhibition of these cells could represent a potential therapeutic approach for excessive scarring and fibrotic diseases like scleroderma.






