Measures of Lung Function Sensitive to Comorbidity of Scleroderma
Accurately determining functional impairment of the respiratory system of scleroderma patients is essential to helping their recovery from symptoms. It is especially important to scleroderma patients with interstitial lung disease and pulmonary arterial hypertension associated with their scleroderma, as their lung function is typically much worse than unaffected scleroderma patients.
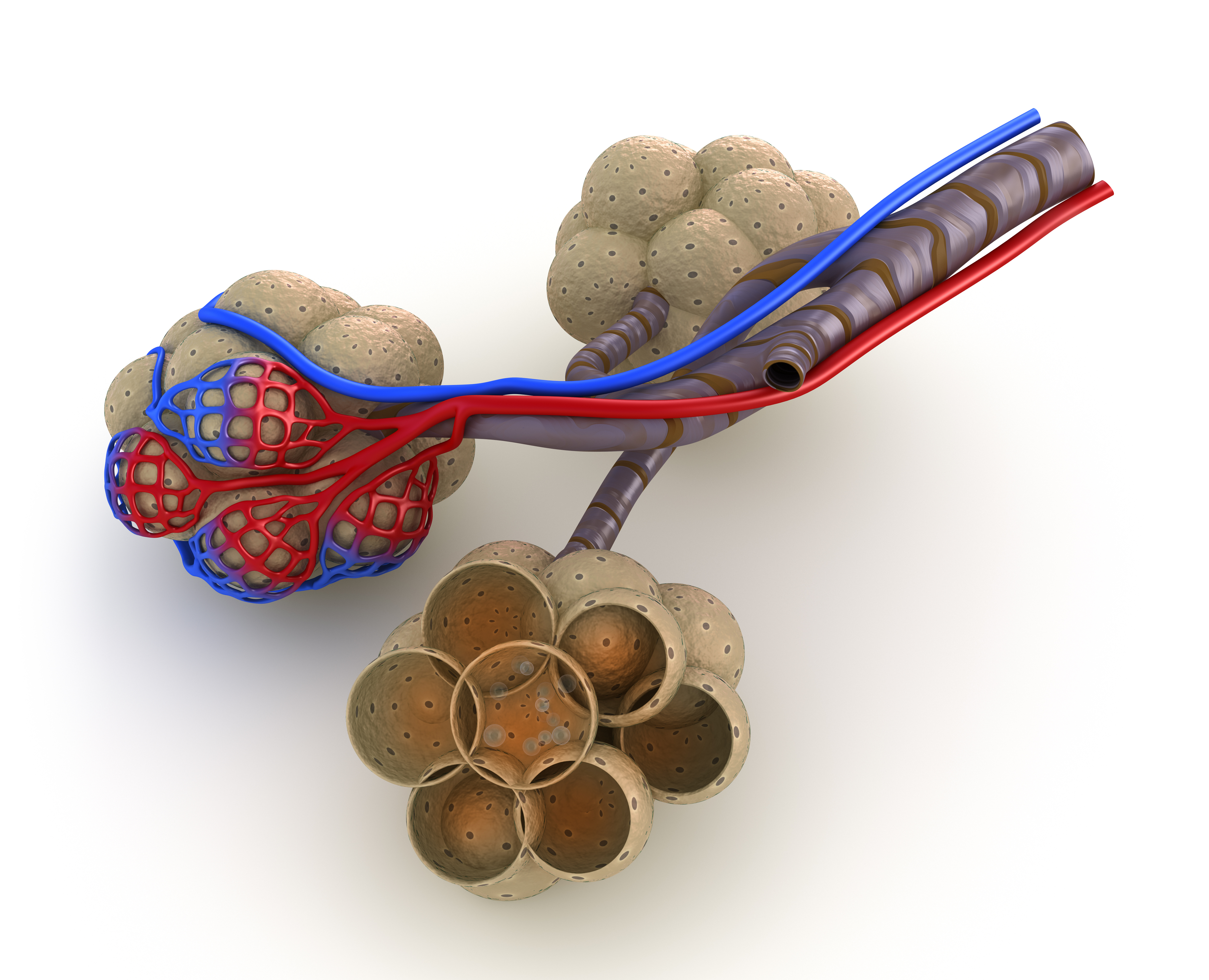
One parameter used to determine lung function is lung diffusing capacity for carbon monoxide (DLCO). This measure is reduced in patients with interstitial lung disease and pulmonary arterial hypertension. However, researchers were unsure if the cause for decreased DLCO was similar between scleroderma patients with either interstitial or vascular involvement of their lungs.
A group from the Department of Cardiologic, Thoracic, and Vascular Sciences at the University of Padua in Italy conducted a study entitled, “Determinants of Impairment in Lung Diffusing Capacity in Patients with Systemic Sclerosis,” and published in the journal Clinical and Experimental Rheumatology. This article looked at DLCO measurements in 37 scleroderma patients and 21 healthy controls. Seventeen of the patients had no pulmonary involvement, and 20 patients had interstitial lung disease with or without pulmonary arterial hypertension. Additional measures for comparison included alveolar-capillary membrane conductance (Dm), pulmonary capillary blood volume (Vc), and diffusing capacity of the lung for nitric oxide (DLNO).
The researchers identified a reduced DLNO and Dm across scleroderma patients compared to controls, but Vc was not affected. Vc was affected when scleroderma patients were split into interstitial lung disease and no pulmonary involvement: those with interstitial lung disease had a significant decrease in both Dm and Vc compared to scleroderma patients and controls, and the difference was most dramatic in those interstitial lung disease patients with pulmonary arterial hypertension.
Interestingly, DLNO was a more sensitive predictor of impaired lung function in scleroderma patients when there were no signs of radiologic or haemodynamic alterations. This result is consistent with previous studies of patients with parenchymal lung disease and pulmonary arterial hypertension. In these patients, the ratio between DLNO/DLCO was useful in identifying pulmonary arterial hypertension, but the ratio could not be used to conduct a differential diagnosis because the overlap between patients with pulmonary arterial hypertension and diffuse parenchymal lung disease. According to the article, “Diffusing Capacity for Nitric Oxide and Carbon Monoxide in Patients with Diffuse Parenchymal Lung Disease and Pulmonary Arterial Hypertension,” which was published in the journal Chest, DLNO represents the true membrane diffusing capacity of the lungs because nitric oxide binds more strongly to hemoglobin and is independent of Vc.
[adrotate group=”3″]
“A disproportional reduction of Dm relative to Vc suggests a thickening of the blood-gas diffusion barrier in these patients,” concluded the authors. “In [scleroderma] patients with detectable interstitial lung disease, the gas exchange impairment is due to both components of lung diffusing capacity, and partitioning of DLCO in Dm and Vc is of little use in distinguishing the patients with only interstitial lung disease from those with interstitial lung disease complicated by pulmonary arterial hypertension.” Another parameter such as DLNO would thus be more appropriate to delineate the two diseases.






