Stem Cell Transplantation Benefits 94% of Diffuse Cutaneous SSc Patients
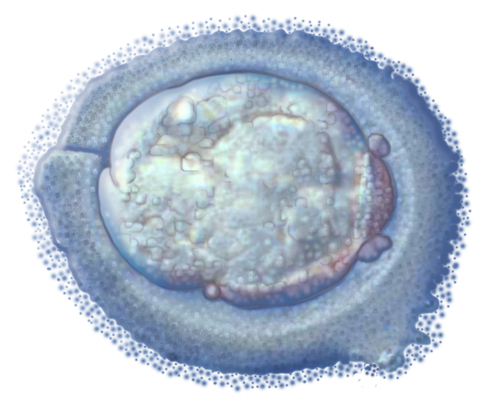
 Recently, autologous haematopoietic stem cell transplantation (AHSCT) has become more popular in treating patients with systemic sclerosis (SSc). Canadian SSc patients have actually been seeking out experimental AHSCT treatments in the United States to aid their recovery from the disease. Despite the popularity, the limited number of clinical trials has prevented researchers from investigating long-term outcomes of AHSCT in patients with severe diffuse cutaneous SSc.
Recently, autologous haematopoietic stem cell transplantation (AHSCT) has become more popular in treating patients with systemic sclerosis (SSc). Canadian SSc patients have actually been seeking out experimental AHSCT treatments in the United States to aid their recovery from the disease. Despite the popularity, the limited number of clinical trials has prevented researchers from investigating long-term outcomes of AHSCT in patients with severe diffuse cutaneous SSc.
A group from UOC Day Hospital Reumatologia in Milano, Italy, under the leadership of Dr. Eleonora Zaccara and Dr. Nicoletta Del Papa, was intrigued by the long-term efficacy of AHSCT and conducted a retrospective study of its use in severe diffuse cutaneous SSc. The findings were presented in”Efficacy of Autologous Hematopoietic Stem Cell Transplantation in Rapidly Progressive Systemic Sclerosis: Prolonged Remission of Disease Activity in a Long-Term Follow Up,” at the American College of Rheumatology 2014 Meeting.
The authors were able to identify literature for 18 patients with diffuse cutaneous SSc who underwent AHSCT. Five males and 13 females were described, with an age range of 20-62 years old. Modified Rodnan Skin Score (mRSS), European Scleroderma Study Group (ESSG) score, organ involvement, and pulmonary function were used as metrics for long-term outcomes.
At the time of follow-up (median was 37 months), 94% of patients demonstrated a beneficial clinical response. Mean mRSS and mean ESSG decreased significantly, and organ involvement was nearly unchanged. Functional respiratory parameters–diffusing capacity of the lung for carbon monoxide (DLCO) and vital capacity (VC)–were similar to baseline levels, and no changes in echocardiography were detected.
It is noted two patients died in the follow-up period as a result of pulmonary and cardiac complications, not from the treatment itself. One patient died as a result of treatment, giving a treatment-related mortality (TRM) of 5.6%. This patient had interstitial pneumonia and died 65 days after treatment.
“This study confirms that AHSCT in selected patients with rapidly progressive SSc results in sustained improvement of skin thickening and stabilization of organ function up to 10 years after transplantation,” wrote the authors in the abstract for the conference. “These findings are in keeping with the view that AHSCT is effective in improving the active phase of SSc, while letting unchanged and stable the fibrosclerotic one.”






